Finance
How Much Does Cosentyx Cost With Insurance?
Published: November 20, 2023
Discover the cost of Cosentyx with insurance coverage. Learn about financing options for this medication and find out how to manage your healthcare expenses.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for LiveWell, at no extra cost. Learn more)
Table of Contents
- Introduction
- Understanding Cosentyx
- The Role of Insurance in Cosentyx Costs
- Factors Affecting Cosentyx Costs with Insurance
- Coverage and Reimbursement Options for Cosentyx
- Typical Insurance Coverage for Cosentyx
- Co-pays and Deductibles for Cosentyx
- Cost-saving Programs for Cosentyx
- Tips for Reducing Cosentyx Costs with Insurance
- Conclusion
Introduction
Welcome to our guide on the cost of Cosentyx with insurance. If you or someone you know is considering or currently using Cosentyx, understanding its cost can be a crucial factor in making informed decisions. Cosentyx is a prescription medication used to treat various inflammatory conditions, including psoriasis, psoriatic arthritis, and ankylosing spondylitis. While it can provide significant relief for those suffering from these conditions, it’s essential to consider the financial aspect.
Insurance coverage plays a significant role in determining the out-of-pocket costs for Cosentyx. Depending on your insurance plan, the terms and conditions of coverage can vary widely. In this article, we will explore the different factors that can affect the cost of Cosentyx with insurance, as well as options for coverage and cost-saving programs.
Understanding and navigating the world of insurance and medications can be overwhelming, but our goal is to provide you with the information and tools you need to make the most cost-effective decisions regarding your treatment with Cosentyx.
Before we delve into the specifics of Cosentyx costs and insurance coverage, let’s take a closer look at what this medication is and how it works.
Understanding Cosentyx
Cosentyx, also known by its generic name secukinumab, is a biologic drug that belongs to a class of medications called interleukin inhibitors. It works by targeting and blocking specific proteins in the immune system that are responsible for causing inflammation.
This medication is primarily used to treat chronic inflammatory conditions, including psoriasis, psoriatic arthritis, and ankylosing spondylitis. Psoriasis is a skin condition characterized by red, itchy, and scaly patches, while psoriatic arthritis affects the joints and can cause pain, stiffness, and swelling. Ankylosing spondylitis is a type of arthritis that primarily affects the spine and can lead to chronic pain and stiffness.
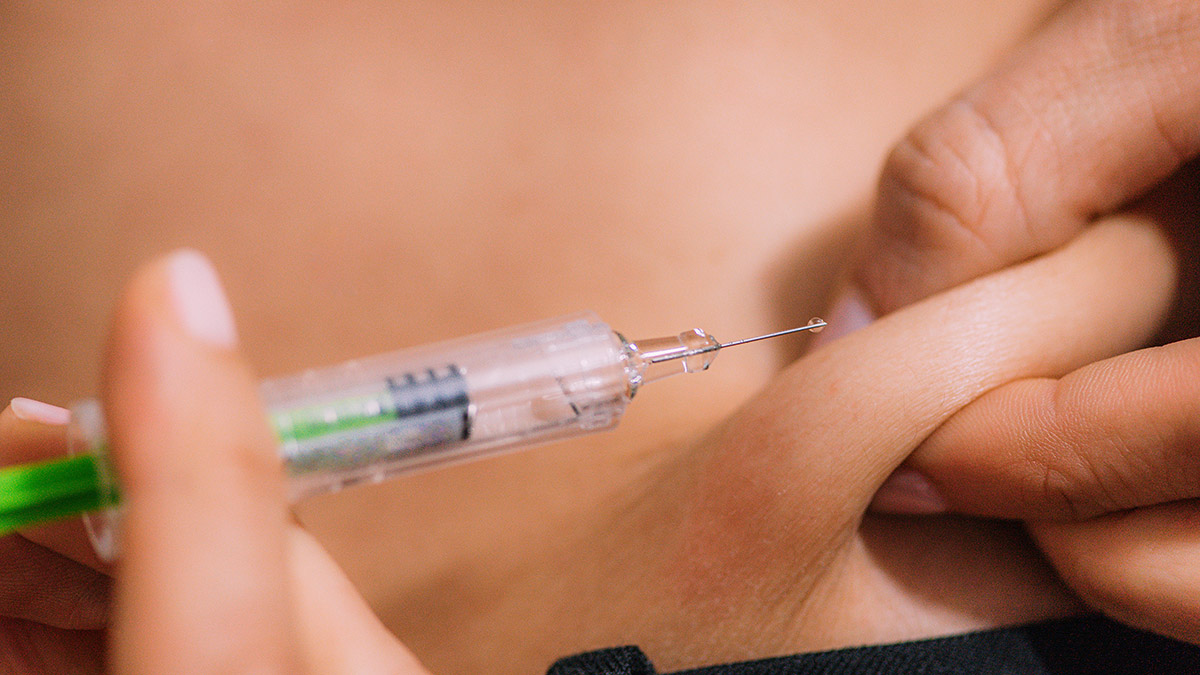
Cosentyx is administered through self-injection, allowing patients to conveniently administer the medication at home after receiving proper training from their healthcare provider. The frequency and dosage of injections may vary depending on the specific condition being treated and the severity of the symptoms.
It’s important to note that Cosentyx is a prescription medication and should only be prescribed by a qualified healthcare professional. If you believe that Cosentyx may be a suitable treatment for your condition, it’s essential to consult with your doctor to undergo a thorough evaluation and discussion of the potential benefits and risks.
Now that we have a basic understanding of Cosentyx let’s delve into the role insurance plays in determining its cost.
The Role of Insurance in Cosentyx Costs
Insurance coverage plays a crucial role in determining the out-of-pocket costs for Cosentyx. The cost of this medication can be quite high, especially without insurance. However, with proper insurance coverage, the expenses can be significantly reduced, making it more affordable for patients.
When it comes to insurance coverage for Cosentyx, it’s important to understand the different types of insurance plans available. This includes private insurance, employer-sponsored plans, Medicare, and Medicaid. Each plan may have different coverage policies and formularies, which is a list of approved medications and their coverage levels.
Under most insurance plans, Cosentyx will fall under the category of specialty drugs. These drugs are often expensive due to their advanced research and complex manufacturing processes. Cosentyx, being a biologic medication, requires careful handling and storage, which adds to its overall cost.
Insurance plans typically require patients to pay a portion of the medication’s cost, known as a co-payment or co-insurance. The specific amount will vary depending on the insurance plan and the tier in which Cosentyx falls within the formulary. Higher-tier medications usually have higher patient responsibility costs.
In addition to co-payments, patients may also have to meet an annual deductible before insurance coverage kicks in. The deductible is the amount that a patient must pay out of pocket before the insurance plan starts contributing to the cost of medications. Once the deductible is met, the patient’s responsibility may shift to a percentage-based co-insurance or a fixed co-payment.
It’s crucial to review the details of your insurance plan to understand the specific coverage and costs for Cosentyx. This can typically be found in the plan’s drug formulary or by contacting your insurance provider directly. Understanding the terms and coverage specifics will help you anticipate and plan for the financial responsibility associated with this medication.
Next, we will explore the various factors that can influence the cost of Cosentyx with insurance.
Factors Affecting Cosentyx Costs with Insurance
Several factors can influence the cost of Cosentyx with insurance. Understanding these factors can help you better navigate the financial aspect of your treatment and potentially find ways to reduce your out-of-pocket expenses.
Insurance Plan Tier: Most insurance plans have tiered formularies, with different medications placed in different tiers. These tiers determine the level of coverage and cost-sharing for the drug. Cosentyx may fall into a higher tier, which often results in higher patient responsibility costs.
Insurance Provider: Different insurance providers may negotiate different discounts and reimbursement rates with pharmaceutical companies. This can impact the cost of Cosentyx with insurance, as the negotiated rate determines the amount the insurance company will cover.
Pharmacy Network: Insurance plans have partnerships with specific pharmacies, which may offer discounted rates for medications like Cosentyx. Utilizing an in-network pharmacy can help reduce your out-of-pocket costs.
Plan Deductible and Co-insurance: If your insurance plan has a high deductible or co-insurance, you may be responsible for a larger portion of the medication cost until the deductible is met. Once the deductible is satisfied, your co-insurance rate will determine the percentage of the medication cost you need to cover.
Patient Assistance Programs: Some pharmaceutical companies offer patient assistance programs to help reduce the cost of their medications for eligible patients. These programs may provide financial assistance or offer co-payment assistance, making Cosentyx more affordable for those who qualify.
Prior Authorization Requirements: Insurance plans may require prior authorization for medications like Cosentyx. This means that your healthcare provider needs to submit additional information to the insurance company to demonstrate the medical necessity of the drug. The process can result in delays and administrative hurdles, impacting access to the medication.
Step Therapy: Some insurance plans may implement step therapy protocols, where patients must try and fail less expensive medications before gaining access to Cosentyx. This can result in delays in starting Cosentyx treatment or additional costs associated with trying alternative medications first.
Understanding these factors and how they can impact the cost of Cosentyx with insurance is essential. By being proactive and informed, you can work with your healthcare provider and insurance company to find the most cost-effective options without compromising the quality of your treatment.
Next, we will explore the coverage and reimbursement options for Cosentyx that may help alleviate some of the financial burden.
Coverage and Reimbursement Options for Cosentyx
When it comes to coverage and reimbursement options for Cosentyx, there are several avenues to explore that can help reduce the financial burden of the medication.
Private Insurance: If you have private health insurance, it is essential to review your plan’s drug formulary to understand the coverage details for Cosentyx. Some insurance plans may require prior authorization or step therapy, while others may cover it without additional requirements. Understanding your plan’s coverage can help you plan for any potential out-of-pocket expenses.
Employer-Sponsored Plans: If you receive insurance coverage through an employer-sponsored plan, it’s important to review the coverage options available. These plans may have different tiers or preferred pharmacies that can impact the cost of Cosentyx. Engaging with your human resources or benefits department can provide valuable insights into available coverage options.
Medicare: For individuals aged 65 and older, or those with certain disabilities, Medicare can provide coverage for Cosentyx. It is important to check whether Cosentyx is covered under Medicare Part B (medical insurance) or Part D (prescription drug coverage). Medicare Part D plans often have different formularies and co-payment structures, so it’s essential to review the specifics of your plan.
Medicaid: Medicaid provides health insurance coverage to low-income individuals and families. While coverage and eligibility can vary by state, Medicaid may cover Cosentyx for eligible patients. It’s important to check with your state’s Medicaid program to understand the coverage criteria and requirements.
Patient Assistance Programs: Pharmaceutical companies that manufacture Cosentyx may offer patient assistance programs to help eligible individuals access the medication at a reduced cost or even for free. These programs usually have specific eligibility criteria based on income, insurance coverage, and medical need. Contacting the manufacturer or visiting their website can provide information on available patient assistance programs.
Copay Support Programs: Some pharmaceutical companies provide copay support programs to help eligible patients cover the out-of-pocket costs associated with Cosentyx. These programs can help reduce or eliminate co-payment responsibilities, making the medication more affordable. Again, contacting the manufacturer or visiting their website can provide information on available copay support programs.
It’s important to explore these coverage and reimbursement options to find the most financially feasible solution for accessing Cosentyx. Consulting with your healthcare provider and insurance company can provide additional guidance and support in navigating these options.
In the next section, we will discuss the typical insurance coverage for Cosentyx and the associated co-pays and deductibles.
Typical Insurance Coverage for Cosentyx
The typical insurance coverage for Cosentyx can vary depending on the specific insurance plan and its formulary. However, understanding some general patterns can give you a better idea of what to expect in terms of coverage.
Many insurance plans provide coverage for Cosentyx, considering it as a specialty medication. Specialty medications like Cosentyx usually require prior authorization, meaning your healthcare provider needs to submit additional information to demonstrate the medical necessity of the drug.
Once approved, insurance plans may cover a percentage of the cost of Cosentyx, typically ranging from 60% to 90%. This percentage is known as the coverage level or co-insurance. The remaining percentage is the responsibility of the patient.
In addition to co-insurance, insurance plans often have a maximum limit or an out-of-pocket maximum. Once you reach this limit, the insurance company will cover 100% of the medication cost for the rest of the coverage period.
It’s important to note that insurance plans may have a preferred drug list or formulary, which only includes specific medications within a therapeutic class. If Cosentyx is not included in your insurance plan’s formulary, it may not be covered, or it may be placed in a higher tier with a higher co-insurance or co-pay responsibility.
Another factor to consider is whether you have met your deductible for the year. Deductibles are the amount you must pay out-of-pocket before your insurance coverage kicks in. If you have not met your deductible, you may be responsible for the full cost of Cosentyx until the deductible is satisfied.
It’s crucial to review your insurance plan’s drug formulary, coverage levels, and out-of-pocket maximum to fully understand your coverage for Cosentyx. If you have any questions or concerns, reaching out to your insurance provider’s customer service department can provide clarity on your specific policy.
In the next section, we will explore the co-pays and deductibles that may be associated with Cosentyx.
Co-pays and Deductibles for Cosentyx
Co-pays and deductibles are important factors to consider when determining the overall cost of Cosentyx with insurance. These terms refer to the financial responsibility that falls on the patient when accessing the medication.
A co-pay is a fixed amount that you are required to pay for each prescription fill. It is usually a set dollar amount, such as $20 or $50, depending on your insurance plan. The co-pay for Cosentyx can vary, depending on the drug’s placement in your insurance plan’s formulary.
On the other hand, a deductible is the amount of money you must pay out-of-pocket before your insurance coverage kicks in. Deductibles are typically annual, meaning they reset at the beginning of each calendar year or policy term. The deductible amount for Cosentyx can vary based on your insurance plan, and it must be met before your insurance starts covering a portion of the medication cost.
For example, let’s say your insurance plan has a $1,000 deductible for specialty medications like Cosentyx. If the cost of Cosentyx is $500 per month, you will be responsible for the full cost of the medication until you reach the $1,000 deductible. Once the deductible is met, your insurance coverage will begin, and you may be responsible for a co-pay or co-insurance percentage.
It’s important to note that co-pays and deductibles can have a significant impact on the overall cost of Cosentyx. If you have a high deductible, you may need to pay a substantial amount out-of-pocket before your insurance coverage takes effect. On the other hand, if your co-pay is high, you may have a fixed dollar amount to pay for each prescription fill, regardless of the medication’s cost.
Reviewing your insurance plan details will provide visibility into the specific co-pay and deductible amounts for Cosentyx. Understanding these costs can help you plan your budget and explore options for cost-saving programs, as discussed in the following sections.
In the next section, we will discuss various cost-saving programs that can help reduce the financial burden of Cosentyx.
Cost-saving Programs for Cosentyx
Recognizing the high cost of Cosentyx, pharmaceutical companies often offer cost-saving programs to help patients access the medication at a more affordable price. These programs can help alleviate the financial burden and make Cosentyx more accessible for those who need it.
Patient Assistance Programs are designed to assist eligible individuals who may have difficulty affording the cost of their medication, including Cosentyx. These programs are typically income-based and provide financial assistance to qualifying patients. They may cover a portion or even the full cost of Cosentyx, helping to make the medication more affordable.
Copay Assistance Programs are offered by pharmaceutical companies to help patients with their out-of-pocket costs, such as co-pays or co-insurance. These programs can provide financial assistance by reducing or eliminating the patient’s responsibility for Cosentyx. They may provide a co-pay card or voucher that can be presented at the pharmacy to reduce the cost at the point of sale.
Patient Savings Programs allow eligible patients to save money on their prescriptions by providing discounts or rebates on the cost of Cosentyx. These programs can help reduce the amount paid directly by the patient, making the medication more affordable.
Manufacturer Discounts may be available through partnerships between pharmaceutical companies and insurance providers. These discounts can help reduce the overall cost of Cosentyx by providing negotiated lower prices for patients with specific insurance plans.
It’s important to note that these cost-saving programs may have specific eligibility criteria and application processes. It’s recommended to reach out to the manufacturer of Cosentyx or visit their website to learn more about the available programs and how to apply.
Additionally, discussing your financial concerns with your healthcare provider can also be helpful. They may have insights into available resources, alternative treatment options, or information on patient assistance foundations that can provide financial support for specialty medications like Cosentyx.
By exploring cost-saving programs and taking advantage of available resources, you can potentially reduce the financial burden associated with Cosentyx and ensure access to this important medication for your treatment.
In the next section, we will provide some practical tips for reducing Cosentyx costs with insurance.
Tips for Reducing Cosentyx Costs with Insurance
Reducing the cost of Cosentyx with insurance can help make the medication more affordable and accessible. Here are some practical tips to consider:
- Review your insurance plan: Take the time to understand your insurance coverage, including the specific details related to Cosentyx. Look into your plan’s drug formulary, co-pays, deductibles, and coverage levels for specialty medications.
- Explore cost-saving programs: Research and inquire about patient assistance programs, copay assistance programs, and other cost-saving initiatives offered by the manufacturer of Cosentyx. These programs can provide financial relief to eligible patients.
- Utilize in-network pharmacies: Check if your insurance plan has preferred pharmacies where you can obtain Cosentyx at a discounted rate. Using an in-network pharmacy can help reduce your out-of-pocket costs.
- Consider generics or alternatives: Discuss with your healthcare provider if there are any generic alternatives or lower-cost medications that are suitable for your condition. Sometimes, there may be more affordable options available that can still effectively manage your symptoms.
- Optimize prescription fill quantities: Check with your healthcare provider if it’s possible to fill a larger quantity of Cosentyx at once. Sometimes, getting a 90-day supply instead of a 30-day supply can result in cost savings.
- Engage with your healthcare provider: Discuss your financial concerns with your healthcare provider. They may be able to provide guidance, suggest cost-saving strategies, or help you navigate the insurance process more effectively.
- Advocate for coverage: If you encounter challenges with insurance coverage for Cosentyx, work with your healthcare provider to provide any necessary documentation or support to appeal the decision. Sometimes, demonstrating medical necessity can result in a favorable coverage decision.
- Be proactive with insurance renewal: When your insurance plan is up for renewal, evaluate your options and consider switching to a plan with better coverage for Cosentyx if available. This can help ensure more favorable cost-sharing arrangements.
- Research patient assistance foundations: Look into charitable organizations and foundations that provide financial assistance specifically for specialty medications. These foundations can help bridge the gap in coverage for those facing high out-of-pocket costs.
- Stay informed: Keep up-to-date with any changes to your insurance plan’s coverage policies or discounts offered by the manufacturer of Cosentyx. Being aware of updates or new programs can help you take advantage of potential cost-saving opportunities.
By implementing these tips and actively managing your insurance coverage, you can work towards reducing the costs associated with Cosentyx and ensure that this important medication remains accessible for your treatment needs.
Finally, let’s conclude this guide with some key takeaways.
Conclusion
Understanding the cost of Cosentyx with insurance is vital for individuals considering or currently using this medication to manage conditions such as psoriasis, psoriatic arthritis, and ankylosing spondylitis. Insurance coverage plays a significant role in determining the out-of-pocket costs associated with Cosentyx, and being informed about the various factors that influence these costs can help patients make informed decisions.
Factors such as insurance plan tier, provider, pharmacy network, deductibles, and co-pays can all impact the overall cost of Cosentyx with insurance. It is essential to review your insurance plan’s drug formulary, coverage levels, and any cost-sharing obligations to better understand your financial responsibility.
Fortunately, there are several coverage and reimbursement options available for Cosentyx, including private insurance, employer-sponsored plans, Medicare, Medicaid, and patient assistance programs. Exploring these options and potential cost-saving programs offered by the manufacturer can help reduce the financial burden and make Cosentyx more affordable.
Additionally, by considering practical tips such as reviewing your insurance plan, utilizing in-network pharmacies, exploring generic or alternative options, and engaging with your healthcare provider, you can further reduce the costs associated with Cosentyx. Staying informed about changes in coverage policies or the availability of cost-saving programs is also crucial.
Ultimately, the goal is to ensure that individuals who can benefit from Cosentyx have access to this important medication without facing excessive financial strain. By understanding the various factors, exploring coverage options, and implementing practical cost-saving strategies, patients can navigate the financial aspect of Cosentyx and focus on their overall health and well-being.
It is important to consult with your healthcare provider, insurance company, and the manufacturer of Cosentyx to discuss your specific situation and obtain personalized advice regarding insurance coverage and cost-saving opportunities.