Home>Finance>What Is The Last Step In The Medical Billing Cycle?


Finance
What Is The Last Step In The Medical Billing Cycle?
Published: March 7, 2024
The last step in the medical billing cycle is crucial for managing finances and ensuring accurate reimbursement. Learn about the final stage and its impact on healthcare finance.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for LiveWell, at no extra cost. Learn more)
Table of Contents
Introduction
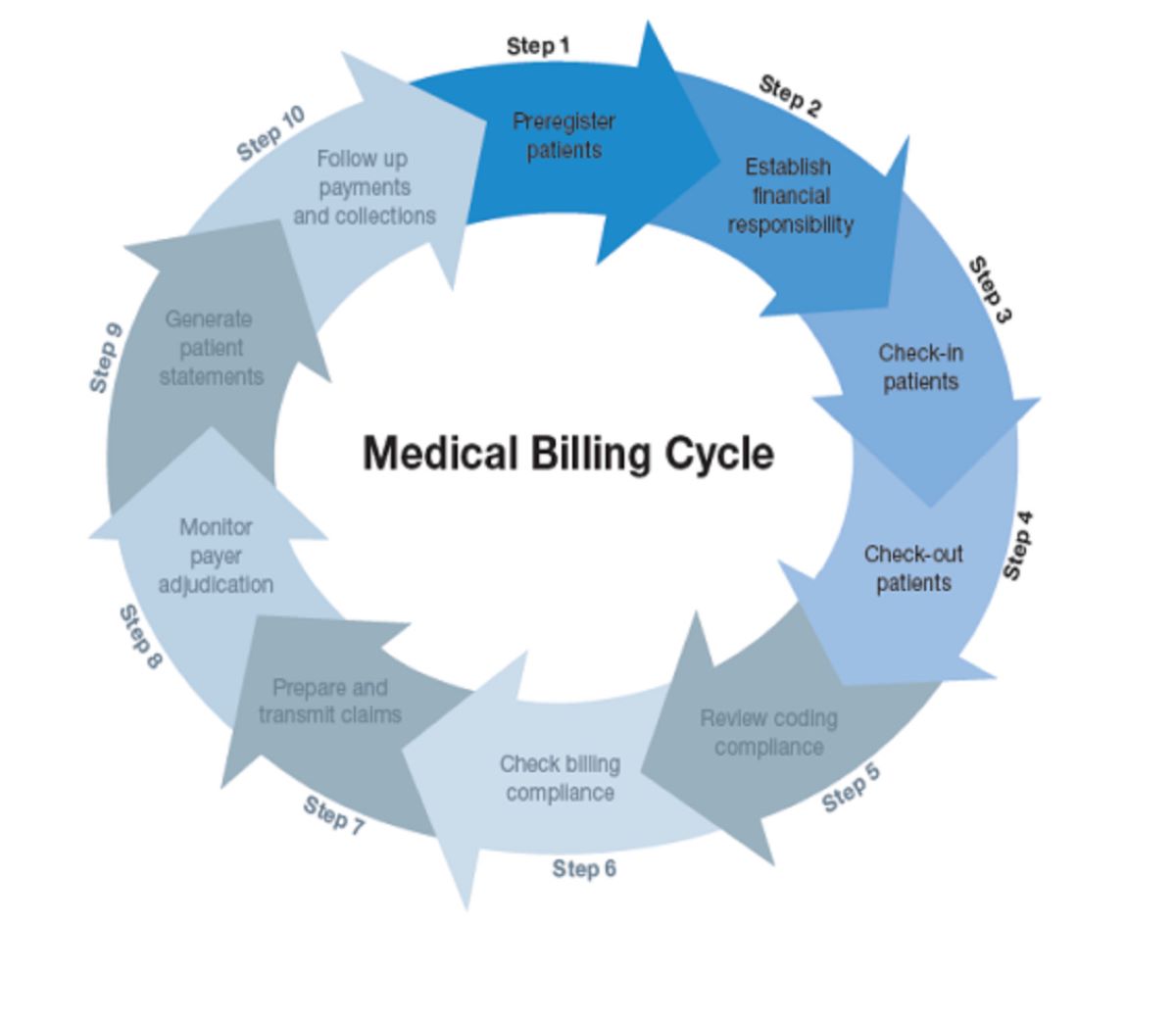
In the complex world of healthcare administration, medical billing plays a crucial role in ensuring that healthcare providers receive proper compensation for their services. The medical billing cycle encompasses a series of steps that begin when a patient makes an appointment and culminate in the healthcare provider receiving payment for the services rendered. Understanding the intricacies of this cycle is essential for healthcare professionals, administrators, and patients alike.
Medical billing involves translating healthcare services into billing claims, which are then submitted to insurance companies or patients for payment. Each step in the medical billing cycle is vital, as errors or oversights at any stage can lead to delays in payment or claim denials. It's crucial for healthcare providers and their administrative staff to navigate this process meticulously to maintain the financial health of the practice and ensure that patients receive the care they need without unnecessary financial burden.
The last step in the medical billing cycle is often overlooked, yet it holds significant importance in ensuring that healthcare providers receive timely and accurate payment for their services. This final stage serves as the bridge between the healthcare provider, the insurance company, and the patient, ultimately facilitating the financial aspect of the care provided.
Understanding the nuances of the last step in the medical billing cycle is essential for healthcare professionals and billing specialists, as it impacts the revenue cycle of the healthcare facility and influences patient satisfaction. In this article, we will delve into the intricacies of the medical billing cycle, explore the significance of its final step, and shed light on why a thorough comprehension of this process is indispensable in the realm of healthcare administration.
Understanding the Medical Billing Cycle
The medical billing cycle is a systematic process that commences when a patient schedules an appointment with a healthcare provider and concludes when the provider receives payment for the services rendered. This intricate sequence of steps involves various stakeholders, including the patient, healthcare provider, insurance companies, and billing specialists.
1. Patient Registration and Check-In: The cycle begins when a patient schedules an appointment with a healthcare provider. During the registration and check-in process, the patient’s demographic and insurance information is collected. This data serves as the foundation for the subsequent billing process.
2. Insurance Verification: Once the patient’s information is gathered, the healthcare facility verifies the patient’s insurance coverage. This step ensures that the services to be provided are covered by the patient’s insurance plan, reducing the likelihood of claim denials due to lack of coverage.
3. Medical Coding: Following the patient’s visit, the healthcare provider documents the services rendered and diagnoses using universally recognized medical codes. Accurate medical coding is crucial, as it directly impacts the reimbursement process by enabling insurance companies to understand the nature of the services provided.
4. Claim Submission: After the medical coding is completed, the billing team compiles the necessary information and submits a claim to the patient’s insurance company. This claim outlines the services provided, associated medical codes, and the amount billed for the services.
5. Adjudication: Upon receiving the claim, the insurance company reviews the information and determines the amount it will pay for the services based on the patient’s coverage and the provider’s contract with the insurance company. This process is known as adjudication.
6. Patient Billing: If there is a remaining balance after the insurance company’s payment, the patient is billed for the outstanding amount. This step involves sending a detailed statement outlining the services provided, the amount covered by insurance, and the patient’s responsibility.
The medical billing cycle is a multifaceted process that requires precision and attention to detail at each stage. Understanding the intricacies of this cycle is paramount for healthcare providers and administrative staff to navigate the complexities of healthcare reimbursement effectively.
The Last Step in the Medical Billing Cycle
The final step in the medical billing cycle involves reconciling the patient’s account and ensuring that the healthcare provider receives the appropriate payment for the services rendered. This critical stage encompasses several key activities that are essential for closing the billing process effectively.
1. Payment Posting: Once the insurance company adjudicates the claim and issues payment, the billing team posts the payment to the patient’s account in the healthcare provider’s financial system. Accurate payment posting is vital to maintain updated and reconciled financial records.
2. Adjustments and Write-Offs: In some cases, the healthcare provider may need to make adjustments or write off a portion of the billed amount. This can occur if the provider has a contractual agreement with the insurance company that necessitates accepting a lower payment as payment in full or if there are specific contractual adjustments based on the provider’s agreement with the insurance company.
3. Patient Communication: After the insurance payment is posted and any necessary adjustments are made, the patient is informed of the remaining balance, if any. Clear and transparent communication regarding the financial responsibility of the patient is crucial for maintaining a positive patient-provider relationship.
4. Resolution of Outstanding Balances: If there is a remaining balance after insurance payment and adjustments, the billing team works to collect the outstanding amount from the patient. This may involve setting up a payment plan or providing guidance on available financial assistance programs.
The last step in the medical billing cycle is pivotal in ensuring that the healthcare provider’s financial records are accurately updated, outstanding balances are resolved, and the revenue cycle is closed effectively. It serves as the final touchpoint in the billing process, solidifying the financial transaction between the healthcare provider, the insurance company, and the patient.
Understanding the intricacies of this last step is crucial for billing specialists and healthcare administrators, as it directly impacts the financial health of the healthcare facility and contributes to overall revenue cycle management. By navigating this stage meticulously, healthcare providers can maintain financial stability and foster positive relationships with their patients.
Importance of the Last Step
The last step in the medical billing cycle holds significant importance for healthcare providers, billing specialists, and patients, playing a pivotal role in ensuring the financial integrity of the healthcare facility and fostering positive patient-provider relationships.
1. Financial Accuracy and Reconciliation: The final step is crucial for maintaining the accuracy of the healthcare provider’s financial records. By posting insurance payments, making necessary adjustments, and resolving outstanding patient balances, the last step ensures that the provider’s financial accounts are reconciled and up to date. This accuracy is essential for financial reporting, auditing, and overall fiscal management.
2. Revenue Cycle Closure: The last step marks the closure of the revenue cycle for the services rendered to the patient. Completing this stage in a timely and accurate manner is vital for the healthcare provider to receive the full and appropriate compensation for the care provided, thereby contributing to the financial sustainability of the practice.
3. Patient Satisfaction and Trust: Clear and transparent communication during the final step of the billing cycle is instrumental in fostering positive patient-provider relationships. Patients appreciate receiving accurate and understandable billing statements, as well as guidance on resolving any outstanding balances. This level of communication contributes to patient satisfaction and helps build trust in the healthcare provider.
4. Compliance and Regulatory Adherence: The last step involves ensuring compliance with regulatory requirements and contractual agreements with insurance companies. Adhering to billing and reimbursement regulations is essential to avoid potential penalties or legal issues, making this stage critical for maintaining the healthcare facility’s compliance with industry standards.
5. Financial Stability and Cash Flow: Effectively navigating the last step in the medical billing cycle contributes to the overall financial stability and cash flow of the healthcare provider. By promptly resolving outstanding balances and accurately recording payments and adjustments, the provider can maintain a healthy revenue cycle and mitigate potential financial challenges.
Understanding the importance of the last step in the medical billing cycle is paramount for healthcare administrators and billing specialists. By recognizing the impact of this stage on financial accuracy, revenue cycle closure, patient satisfaction, regulatory compliance, and financial stability, healthcare providers can prioritize the meticulous execution of the final phase of the billing process.
Conclusion
The medical billing cycle is a multifaceted process that culminates in the last step, which holds significant importance for healthcare providers, billing specialists, and patients. Understanding the intricacies of this final phase is essential for maintaining the financial integrity of the healthcare facility, fostering positive patient-provider relationships, and ensuring compliance with regulatory standards.
By navigating the last step meticulously, healthcare providers can achieve several critical outcomes. Financial accuracy and reconciliation are upheld through the posting of insurance payments, adjustments, and resolution of outstanding patient balances. This precision contributes to the provider’s fiscal management, compliance with industry standards, and the closure of the revenue cycle for services rendered.
Moreover, the last step plays a pivotal role in nurturing patient satisfaction and trust. Clear and transparent communication regarding billing statements and outstanding balances fosters positive patient-provider relationships, enhancing the overall patient experience. Additionally, the effective execution of this stage contributes to the healthcare provider’s financial stability, cash flow management, and adherence to contractual agreements with insurance companies.
As the healthcare landscape continues to evolve, the significance of the last step in the medical billing cycle remains paramount. Billing specialists and healthcare administrators must prioritize a comprehensive understanding of this phase to navigate the complexities of healthcare reimbursement effectively. By recognizing the impact of the last step on financial accuracy, revenue cycle closure, patient satisfaction, compliance, and financial stability, healthcare providers can ensure the seamless and efficient conclusion of the medical billing process.
In conclusion, the last step in the medical billing cycle serves as the linchpin that solidifies the financial transaction between the healthcare provider, the insurance company, and the patient. Its meticulous execution is indispensable for the financial health of the healthcare facility and the overall satisfaction of patients, highlighting its integral role in the realm of healthcare administration.