Home>Finance>How Do Coding And Billing Cycle Processes Impact Healthcare Organization Revenue Cycles?
Finance
How Do Coding And Billing Cycle Processes Impact Healthcare Organization Revenue Cycles?
Published: March 7, 2024
Learn how the coding and billing cycle processes affect healthcare organization revenue cycles and financial performance. Explore the impact of finance on revenue management.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for LiveWell, at no extra cost. Learn more)
Table of Contents
Introduction
In the complex ecosystem of healthcare organizations, the efficient management of revenue cycles is paramount for financial stability and the delivery of quality patient care. At the heart of this intricate process lie the coding and billing cycle processes, which play a pivotal role in determining the financial health of healthcare providers. Understanding the interplay between coding, billing, and revenue cycles is essential for healthcare professionals, administrators, and stakeholders to optimize operational efficiency and financial performance.
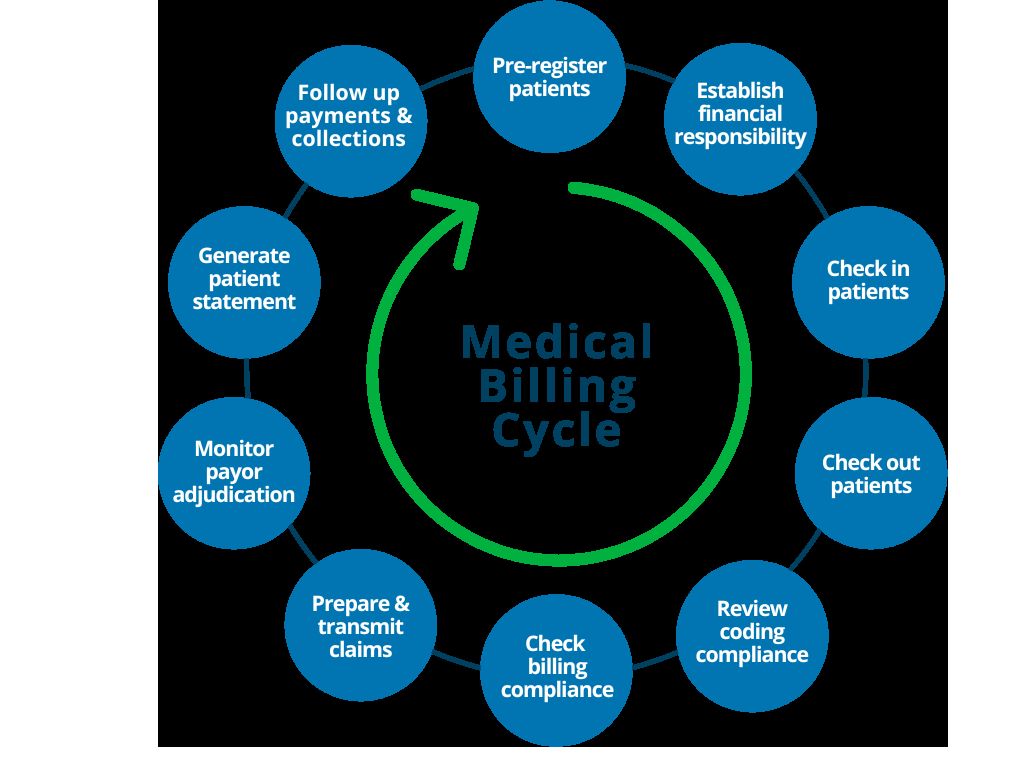
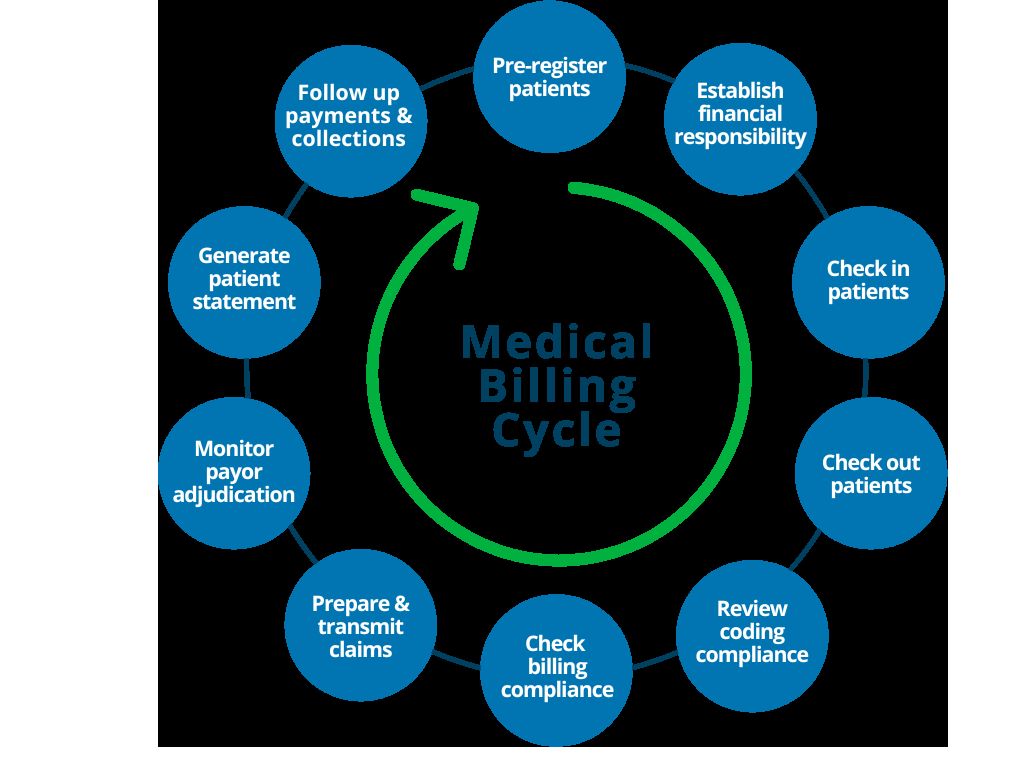
The coding and billing cycle processes encompass a series of interconnected activities that begin with documenting patient encounters and culminate in the reimbursement of services rendered. These processes are not only crucial for ensuring accurate and timely payments but also for maintaining compliance with regulatory requirements and industry standards. Moreover, they directly influence the overall revenue cycle, impacting the financial viability of healthcare organizations.
By delving into the intricacies of the coding and billing cycle processes, healthcare professionals can gain valuable insights into the factors that shape revenue cycles. This comprehensive understanding empowers organizations to implement strategic initiatives aimed at enhancing revenue integrity, reducing claim denials, and mitigating compliance risks. Consequently, a well-optimized coding and billing framework can bolster the financial sustainability of healthcare entities while fostering a seamless and efficient patient care continuum.
As we navigate through the nuances of coding, billing, and revenue cycles, it becomes evident that the synergy between these elements is instrumental in driving operational excellence and financial prosperity within the healthcare landscape. Through this exploration, we aim to unravel the multifaceted impact of coding and billing processes on revenue cycles, shedding light on the strategies that can be employed to optimize these critical functions.
Understanding the Coding Process
The coding process in healthcare involves the transformation of diagnoses, procedures, and services into universally recognized alphanumeric codes. These codes are integral to the billing and reimbursement cycle, as they convey vital information about patient encounters, treatments, and medical interventions. At its core, accurate coding ensures that healthcare services are appropriately documented and classified, laying the foundation for transparent communication among healthcare providers, payers, and regulatory bodies.
Healthcare coding encompasses two primary code sets: the International Classification of Diseases (ICD) codes and the Current Procedural Terminology (CPT) codes. ICD codes capture diagnoses and medical conditions, providing a standardized framework for classifying ailments and illnesses. On the other hand, CPT codes delineate medical procedures and services, offering a comprehensive taxonomy of billable healthcare activities. By meticulously assigning the relevant codes to patient encounters, healthcare professionals facilitate the accurate reporting and billing of services, thereby ensuring proper reimbursement for the care delivered.
Furthermore, the coding process demands a deep understanding of medical terminology, disease pathology, and treatment modalities. This proficiency enables coders to decipher complex medical records, interpret physician documentation, and translate clinical narratives into precise codes. Moreover, coding professionals must stay abreast of evolving healthcare regulations and coding guidelines to maintain compliance and uphold the integrity of the coding process.
Effective coding not only serves as a cornerstone of revenue cycle management but also supports clinical decision-making, population health management, and healthcare analytics. By harnessing the power of coded data, healthcare organizations can derive actionable insights, identify trends in patient populations, and streamline care delivery processes. Additionally, accurate coding facilitates the aggregation of clinical data for research, quality reporting, and epidemiological studies, thus contributing to advancements in medical knowledge and public health initiatives.
In essence, the coding process is a linchpin of healthcare operations, bridging the realms of clinical care and financial stewardship. Its significance reverberates across the entire healthcare ecosystem, underscoring the critical role it plays in shaping revenue cycles and ensuring the efficient functioning of healthcare organizations.
The Importance of Accurate Billing
Accurate billing is the bedrock of financial solvency for healthcare organizations. It encompasses the precise generation and submission of claims for the services rendered to patients, insurers, and government payers. A meticulous billing process ensures that healthcare providers receive rightful compensation for the care they deliver, thereby fortifying the revenue streams essential for sustaining operations and fostering continuous improvement in patient care.
At the crux of accurate billing lies the translation of coded data into comprehensive claims that adhere to the specific requirements of diverse payers. This entails crafting detailed and compliant claims that encapsulate the scope and specifics of patient encounters, treatments, and interventions. Moreover, accurate billing necessitates a nuanced understanding of payer policies, reimbursement methodologies, and regulatory mandates, as deviations from these guidelines can lead to claim denials, delayed payments, or potential compliance issues.
Furthermore, precise billing practices are instrumental in fostering transparency and trust between healthcare providers and payers. By submitting accurately documented claims, organizations demonstrate their commitment to ethical billing standards and compliance with industry regulations, thereby enhancing their credibility and fostering positive relationships with payers. This, in turn, can expedite the reimbursement process and minimize disputes, contributing to a more seamless revenue cycle and improved financial performance.
From a patient perspective, accurate billing plays a pivotal role in promoting transparency and understanding of healthcare costs. Clear and accurate billing statements empower patients to comprehend the financial aspects of their care, make informed decisions regarding treatment options, and navigate the complexities of insurance coverage. By fostering transparency and clarity in billing, healthcare organizations can engender trust and satisfaction among patients, thereby bolstering their reputation and patient retention rates.
Ultimately, the importance of accurate billing extends beyond financial considerations, permeating every facet of healthcare delivery. It upholds the integrity of revenue cycles, nurtures trust among stakeholders, and reinforces the ethical underpinnings of healthcare operations. By prioritizing accuracy in billing processes, healthcare organizations can fortify their financial foundations, cultivate positive relationships with payers and patients, and sustainably drive their mission of providing high-quality, accessible care to the communities they serve.
Impact of Coding and Billing on Revenue Cycle
The symbiotic relationship between coding, billing, and the revenue cycle is pivotal in shaping the financial health of healthcare organizations. The accuracy and efficiency of coding and billing processes directly influence the entire revenue cycle, spanning from patient registration to the final collection of payments. A seamless integration of these functions is essential to optimize revenue cycle management and ensure the sustained financial viability of healthcare entities.
Effective coding and billing practices lay the groundwork for streamlined revenue cycle operations. By accurately translating clinical encounters and services into coded data and subsequently crafting precise claims, healthcare organizations expedite the billing and reimbursement process. This, in turn, accelerates the inflow of revenue, minimizes accounts receivable aging, and bolsters the liquidity necessary for sustaining day-to-day operations and strategic growth initiatives.
Conversely, inaccuracies or inefficiencies in coding and billing can trigger cascading effects throughout the revenue cycle. Incorrectly coded encounters, erroneous claims, or billing discrepancies can lead to claim denials, payment delays, and revenue leakage. Such disruptions not only impede the cash flow of healthcare organizations but also necessitate additional resources for claims rework, appeals, and compliance rectification, thereby straining operational efficiency and financial resources.
Moreover, the impact of coding and billing resonates beyond the financial realm, permeating the overall patient experience and organizational reputation. Inaccurate billing or coding errors can result in patient dissatisfaction, erode trust in the healthcare provider, and tarnish the organization’s standing in the community. Conversely, seamless coding and billing processes contribute to a positive patient financial experience, fostering trust and loyalty while reinforcing the organization’s commitment to operational excellence.
Furthermore, the interplay between coding, billing, and the revenue cycle is instrumental in facilitating data-driven decision-making and performance analysis. Accurate coded data and billing information serve as valuable inputs for revenue cycle analytics, enabling healthcare organizations to identify trends, pinpoint areas for improvement, and implement targeted strategies to enhance financial performance and operational efficiency.
In essence, the impact of coding and billing on the revenue cycle is profound and multifaceted. By recognizing the interconnectedness of these functions and implementing measures to optimize their synergy, healthcare organizations can fortify their financial foundations, elevate the patient experience, and navigate the complexities of the evolving healthcare landscape with resilience and agility.
Strategies for Improving Coding and Billing Processes
Enhancing coding and billing processes is imperative for optimizing revenue cycle management and fortifying the financial sustainability of healthcare organizations. By implementing strategic initiatives aimed at refining coding and billing functions, healthcare entities can mitigate compliance risks, minimize revenue leakage, and bolster operational efficiency. Several key strategies can be employed to elevate the performance of coding and billing processes:
- Continuous Staff Training and Education: Investing in ongoing training programs for coding and billing staff is essential to ensure proficiency in evolving coding guidelines, regulatory requirements, and industry best practices. Equipping staff with updated knowledge and skills fosters accuracy and compliance in coding and billing activities.
- Utilization of Technology and Automation: Leveraging advanced coding and billing software solutions can streamline processes, reduce errors, and enhance productivity. Automation tools can facilitate accurate code assignment, claims generation, and billing accuracy, thereby optimizing operational efficiency and accelerating revenue cycles.
- Regular Audits and Quality Assurance: Conducting routine audits of coding and billing processes can uncover discrepancies, identify areas for improvement, and ensure adherence to regulatory standards. Implementing robust quality assurance protocols safeguards against errors and mitigates compliance risks.
- Collaboration and Communication: Fostering seamless communication and collaboration between coding, billing, and clinical teams is essential for ensuring accurate documentation and code assignment. By promoting interdisciplinary cooperation, healthcare organizations can enhance the accuracy and completeness of coded data, thereby fortifying the revenue cycle.
- Comprehensive Documentation and Clinical Integration: Encouraging thorough and precise clinical documentation by healthcare providers is pivotal for accurate code assignment and billing. Integration of coding and billing considerations into clinical workflows promotes a holistic approach to healthcare data management, ensuring the integrity and accuracy of coded information.
- Compliance Monitoring and Adherence: Establishing robust compliance monitoring mechanisms and fostering a culture of adherence to coding and billing regulations is critical. By prioritizing compliance, healthcare organizations can mitigate the risk of audits, penalties, and reputational damage while upholding ethical billing practices.
By embracing these strategies and cultivating a culture of continuous improvement, healthcare organizations can optimize their coding and billing processes, fortify revenue cycle management, and navigate the complexities of the healthcare landscape with resilience and agility.
Conclusion
The intricate interplay between coding, billing, and the revenue cycle constitutes a fundamental axis that underpins the financial health and operational efficiency of healthcare organizations. The seamless integration of these processes is essential for optimizing revenue cycle management, ensuring accurate reimbursement, and fostering trust among stakeholders. By delving into the nuances of coding and billing, healthcare professionals and administrators gain valuable insights into the pivotal role these functions play in shaping the financial landscape of healthcare.
Effective coding and billing practices not only expedite the revenue cycle but also promote transparency, compliance, and patient-centric financial experiences. Accurate coding ensures that clinical encounters are meticulously documented and classified, providing the foundation for precise billing and claims generation. This, in turn, fosters trust and transparency in financial transactions, empowering patients to navigate the complexities of healthcare costs with clarity and confidence.
Furthermore, the impact of coding and billing reverberates beyond financial considerations, permeating the overall patient experience and organizational reputation. Accurate coding and billing practices contribute to a positive patient financial journey, fostering trust, satisfaction, and loyalty. By prioritizing accuracy and compliance in these processes, healthcare organizations elevate the quality of care delivery and fortify their standing in the communities they serve.
As healthcare continues to evolve, the optimization of coding and billing processes remains a linchpin for financial sustainability and operational excellence. By implementing strategic initiatives such as continuous staff training, technology utilization, and compliance monitoring, healthcare organizations can fortify their coding and billing functions, thereby enhancing revenue cycle management and navigating the complexities of the healthcare landscape with resilience and agility.
In essence, the synergy between coding, billing, and the revenue cycle epitomizes the convergence of clinical care and financial stewardship. By recognizing the profound impact of these processes and embracing strategies for continuous improvement, healthcare organizations can fortify their financial foundations, elevate the patient experience, and uphold the ethical and operational standards that define the essence of healthcare delivery.