Finance
How Much Is STD Test With Insurance?
Published: November 18, 2023
Looking for the cost of an STD test with insurance? Discover how finance plays a crucial role in determining the price with our comprehensive guide.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for LiveWell, at no extra cost. Learn more)
Table of Contents
Introduction
Welcome to the world of finance! Whether you’re just starting on your financial journey or looking to expand your knowledge, understanding the ins and outs of the finance industry is essential. One important aspect of finance that often gets overlooked is the world of insurance. With so many different types of insurance available, it can be challenging to navigate through the complexities. In this article, we will specifically focus on one type of insurance coverage – STD testing insurance coverage.
Sexually transmitted diseases (STDs) are a common occurrence and can have significant health implications if left untreated. Therefore, it is crucial to get tested regularly to ensure early detection and treatment. However, the cost of STD testing can be a concern for many individuals. That’s where insurance coverage comes into play.
Insurance coverage for STD testing varies depending on the type of insurance plan you have and the provider you choose. Understanding the coverage options and associated costs can help you make informed decisions about your health and finances.
Throughout this article, we will explore the different types of STD tests, how insurance providers handle coverage, co-payments and deductibles, in-network vs. out-of-network providers, preauthorization and approval requirements, as well as confidentiality and privacy concerns.
By the end of this article, you’ll have a comprehensive understanding of how much STD testing with insurance might cost you and the factors to consider when seeking coverage for this essential health service.
Understanding STD Testing
Before diving into the details of insurance coverage for STD testing, it is essential to have a basic understanding of what STD testing entails. STD tests are medical procedures performed to detect the presence of sexually transmitted infections in individuals.
There are several types of STDs, including but not limited to chlamydia, gonorrhea, syphilis, herpes, HIV, and hepatitis. Each STD requires a specific test for accurate diagnosis. It is important to note that not all tests are performed in the same way and may vary depending on the type of infection being tested for.
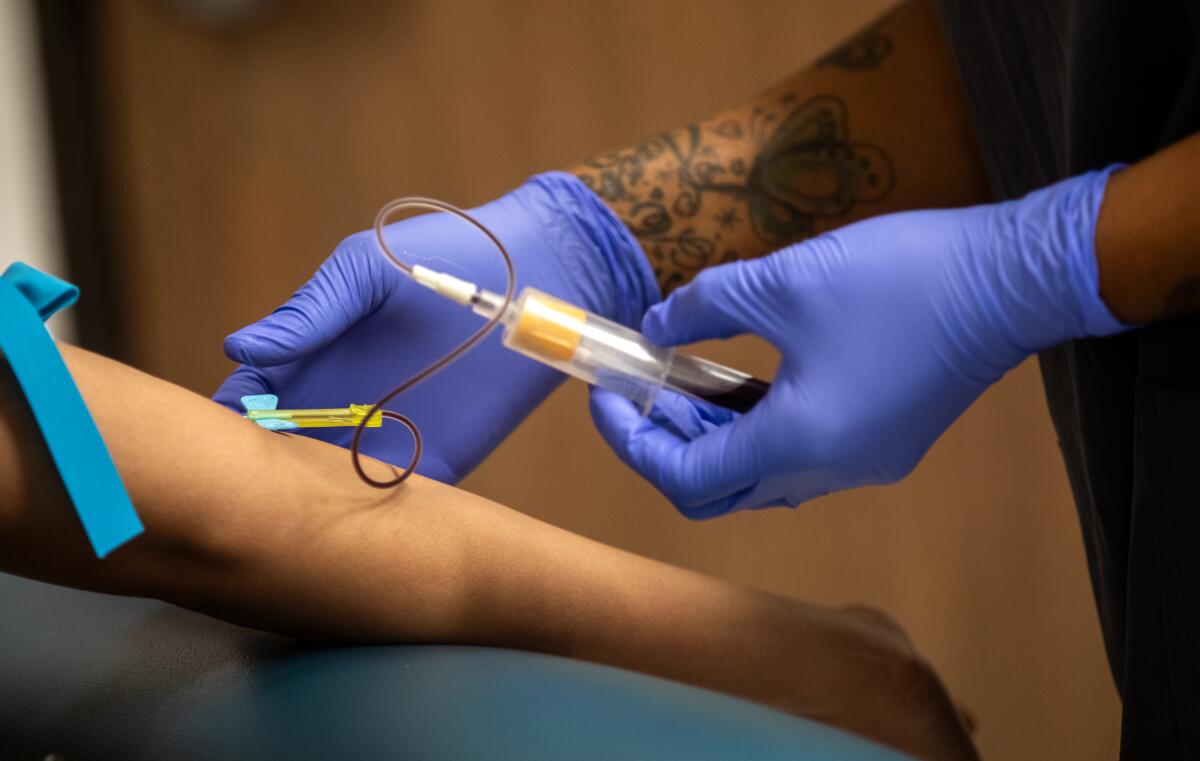
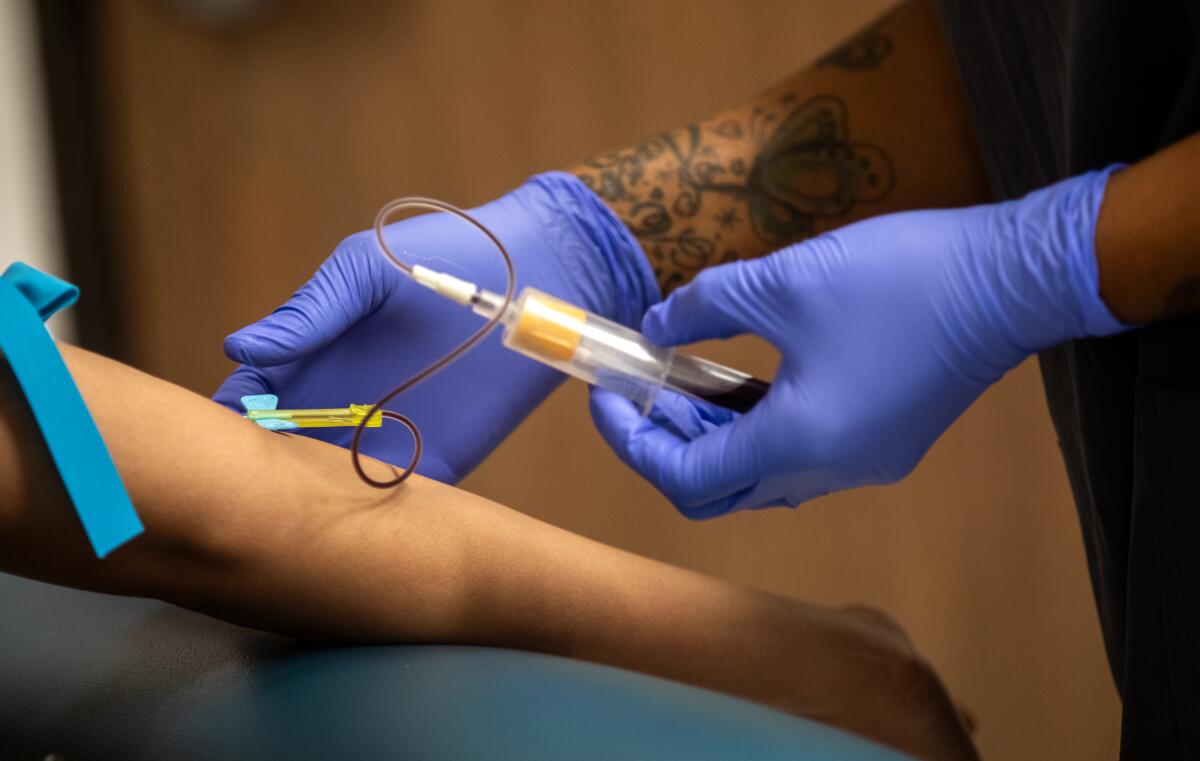
STD testing can involve a range of procedures, including blood tests, urine tests, swab tests, and physical examinations. The specific type of test required will depend on the suspected STD and the recommendations of your healthcare provider.
It is important to seek regular STD testing, especially if you are sexually active or engage in high-risk behaviors. Early detection is key to effective treatment and can help prevent further transmission of infections. Additionally, some STDs may not show any visible symptoms, making testing even more crucial.
STD testing is typically conducted at healthcare facilities, clinics, or specialized testing centers. You can consult with your primary care physician or visit a sexual health clinic to get tested. Some clinics also offer confidential and anonymous testing options to ensure privacy.
Now that we have a better understanding of STD testing, let’s explore how insurance coverage can help offset the costs of these necessary medical procedures.
Coverage for STD Testing
When it comes to insurance coverage for STD testing, each insurance provider and plan may have different policies and guidelines. However, many insurance plans do offer some form of coverage for STD testing.
In general, insurance coverage for STD testing falls under preventive care services. Preventive care aims to detect and prevent illnesses before they become more severe or costly to treat. STD testing is considered a preventive service since early detection of sexually transmitted infections can lead to prompt treatment and reduce the risk of spreading the infection to others.
Under the Affordable Care Act (ACA), most insurance plans are required to cover certain preventive services, including STD testing, without charging a co-payment or deductible. However, it is important to check your specific plan details to confirm what services are covered and if any cost-sharing responsibilities apply.
Insurance coverage for STD testing can vary based on several factors, such as deductibles, co-payments, and whether you choose an in-network or out-of-network provider. Some plans may cover the full cost of STD testing, while others may require you to pay a portion of the cost.
If you have health insurance, the first step is to review your policy documents or contact your insurance provider to understand the specifics of your coverage. It is important to be aware of any limitations, restrictions, or preauthorization requirements before seeking STD testing.
If you don’t have health insurance, there are other options available. Many state and local health departments offer free or low-cost STD testing services. Additionally, there are non-profit organizations and community clinics that provide affordable or sliding-scale fee services for individuals without insurance.
Keep in mind that even with insurance coverage, there may still be certain expenses involved, such as co-payments for office visits or additional tests. It is crucial to understand the details of your insurance coverage to avoid any unexpected costs.
Next, let’s explore the different types of STD tests and their associated costs, which can also influence insurance coverage.
Types of STD Tests and Costs
STD testing involves various types of tests, depending on the suspected infection and the healthcare provider’s recommendations. Here are some common types of STD tests:
- 1. Blood Tests: Blood tests are used to detect certain STDs like HIV, syphilis, and hepatitis. These tests usually involve drawing a small blood sample, which is then sent to a laboratory for analysis. The cost of blood tests can vary depending on the specific tests being performed.
- 2. Urine Tests: Urine tests are frequently used to diagnose infections like chlamydia and gonorrhea. The individual provides a urine sample, which is then analyzed for the presence of the bacteria causing the infection. The cost of urine tests can vary based on the testing method and the specific STD being screened for.
- 3. Swab Tests: Swab tests involve taking samples from the affected area, such as the genitals, rectum, or throat. These samples are then examined for infections like herpes, chlamydia, gonorrhea, or syphilis. Swab tests may require the use of a cotton swab or brush to collect the samples. The cost of swab tests can vary depending on the number of samples taken and the specific STD being tested.
- 4. Physical Examinations: Physical examinations may be required for certain STDs, such as genital warts or genital herpes. During the examination, the healthcare provider visually inspects the affected area to check for any visible signs of infection. The cost of physical examinations can vary depending on the healthcare provider and the specific STD being examined.
The cost of STD tests can vary significantly depending on factors like the type of test, the healthcare provider’s location, and whether you have insurance coverage. Without insurance, the cost of STD testing can range from $50 to several hundred dollars per test, depending on the specific test and the laboratory used.
Fortunately, many insurance plans offer coverage for STD testing, reducing or eliminating the out-of-pocket cost for policyholders. Under the ACA, insurance plans are required to cover certain preventive services, including STD testing, without charging a co-payment or deductible. However, it is crucial to verify with your insurance provider if the specific tests you require are covered and to what extent.
When considering the costs of STD tests, it is essential to consider whether you are visiting an in-network or out-of-network provider. In-network providers have negotiated rates with your insurance company and may offer more affordable options. Out-of-network providers, on the other hand, may charge higher fees, and you may be responsible for a larger portion of the costs.
Now that we have explored the types of STD tests and their associated costs, let’s delve into how insurance providers handle coverage for STD testing.
Insurance Providers and Coverage
Insurance providers play a crucial role in determining the coverage and cost of STD testing. Different insurance companies may have varying policies and guidelines regarding the coverage of preventive services, including STD testing.
Most health insurance plans, including private insurance, employer-sponsored plans, and plans obtained through the Health Insurance Marketplace, offer some level of coverage for STD testing. However, the extent of coverage may differ from plan to plan.
It is important to review your insurance policy documents or contact your insurance provider directly to understand the specifics of your coverage for STD testing. Pay close attention to the services covered, any limitations or exclusions, and any required preauthorization or referral processes.
Many insurance providers follow the guidelines set by the Affordable Care Act (ACA), which requires coverage for certain preventive services without charging a co-payment or deductible. These preventive services include STD testing for sexually active individuals or those at high risk for sexually transmitted infections.
However, it is worth noting that some plans may still impose cost-sharing requirements, such as deductibles, co-payments, or co-insurance. These out-of-pocket expenses may vary depending on the specific plan and the insurance provider.
Additionally, insurance providers often have a network of preferred healthcare providers, referred to as in-network providers. In-network providers have negotiated rates with the insurance company, resulting in lower out-of-pocket costs for policyholders. It is advisable to choose an in-network provider for STD testing to maximize your insurance coverage and minimize your expenses.
If you decide to visit an out-of-network provider, it is important to check with your insurance company regarding the coverage and any additional costs you may incur. Out-of-network providers may not have agreed-upon rates with your insurance company, which could result in higher out-of-pocket expenses for you.
Understanding your insurance provider’s coverage for STD testing is crucial to avoid any unexpected expenses or denial of claims. If you have any doubts or questions, it is always a good idea to reach out to your insurance provider for clarification.
Now, let’s delve into the concepts of co-payments and deductibles, as they play a significant role in determining your financial responsibility for STD testing.
Co-payments and Deductibles
When it comes to insurance coverage for STD testing, co-payments and deductibles are important factors to consider. These are the out-of-pocket expenses that policyholders are responsible for paying when receiving medical services.
A co-payment, or co-pay, is a fixed amount that you pay for each visit or service. For STD testing, you may have a co-payment for the office visit or for each specific test performed. The co-payment amount can vary depending on your insurance plan. Some plans may have a flat co-payment, while others may require a percentage of the total cost of the service.
It is essential to review your insurance policy details to understand the co-payment requirements for STD testing. These details can make a difference in the overall cost of your testing, so it is important to be aware of them in advance.
A deductible is the amount you must pay for medical services before your insurance coverage kicks in. For example, if you have a $500 deductible, you will need to pay the first $500 of covered services out of your own pocket before your insurance begins to cover the remaining costs.
When it comes to STD testing, if the cost of your tests falls below your deductible, you will be responsible for paying the full amount. However, if the cost exceeds your deductible, your insurance should cover the remaining portion according to your policy terms.
It is important to note that deductibles can vary significantly from one insurance plan to another. Some plans may have a low deductible, while others may have a high deductible. Understanding your plan’s deductible is crucial in determining your financial responsibility for STD testing.
Once you have met your deductible, your insurance will typically cover a percentage of the costs of STD testing, and you will be responsible for the remaining percentage, which is known as co-insurance. The percentage paid by your insurance and your co-insurance responsibility will depend on your specific plan.
It’s important to remember that co-payments, deductibles, and co-insurance apply to covered services. If a test or service is not covered by your insurance plan, you will be responsible for the full cost.
Understanding the co-payment and deductible requirements of your insurance plan can help you plan financially for STD testing and determine your out-of-pocket expenses. Now, let’s discuss the concept of in-network and out-of-network providers and the impact they can have on your insurance coverage.
In-Network vs Out-of-Network Providers
When seeking insurance coverage for STD testing, it is important to consider whether the healthcare provider you choose is considered in-network or out-of-network. These terms refer to the relationship between the healthcare provider and your insurance company, and they can have a significant impact on your coverage and out-of-pocket expenses.
An in-network provider refers to a healthcare provider or facility that has a contract or agreement with your insurance company to provide services at pre-negotiated rates. These providers have established relationships with the insurance company, which often results in lower costs for policyholders.
When you visit an in-network provider for STD testing, you can generally expect your insurance coverage to be more comprehensive. The insurance company is more likely to cover a larger portion of the costs, and your out-of-pocket expenses, such as co-payments and deductibles, are typically lower.
On the other hand, an out-of-network provider refers to a healthcare provider or facility that does not have a contract or agreement with your insurance company. These providers may still offer services, but they may not have established rates with your insurance company.
When you receive STD testing from an out-of-network provider, your insurance coverage may be limited, and you may be responsible for a larger portion of the costs. Out-of-network providers can charge higher fees, which can result in higher out-of-pocket expenses for you.
It is crucial to check with your insurance provider to see if a specific healthcare provider is considered in-network. Insurance companies often have directories or online tools that list in-network providers, making it easier for you to find a suitable provider.
It’s worth noting that some insurance plans may provide partial coverage for out-of-network services, but the out-of-pocket expenses are typically higher. It is important to understand the specific terms of your insurance policy regarding out-of-network coverage.
When seeking insurance coverage for STD testing, it is generally recommended to choose an in-network provider whenever possible. This will help ensure that you receive the maximum coverage and minimize your out-of-pocket expenses.
Now that we understand the difference between in-network and out-of-network providers, let’s explore the concept of preauthorization and approval, which can have an impact on the coverage of STD testing.
Preauthorization and Approval
When it comes to insurance coverage for STD testing, preauthorization and approval are important processes that may be required by your insurance provider. These processes ensure that the proposed medical services, including the specific STD tests, meet the criteria for coverage outlined in your insurance policy.
Preauthorization is the process of obtaining approval from your insurance company before receiving certain medical services, including STD testing. The purpose of preauthorization is to ensure that the proposed services are medically necessary and meet the guidelines set by your insurance provider.
It is important to note that not all insurance plans require preauthorization for STD testing. However, many plans do have specific requirements and criteria for preauthorization. It’s essential to review your insurance policy or contact your insurance provider to determine if preauthorization is necessary.
During the preauthorization process, your healthcare provider may need to submit medical documentation and information related to the STD testing. This documentation helps the insurance company determine if the tests are medically necessary and meet the coverage criteria.
If preauthorization is required, it is important to obtain approval from your insurance provider before proceeding with the STD testing. Failing to obtain preauthorization when required can result in the denial of coverage and potential financial responsibility.
It is worth noting that preauthorization requirements and processes can vary among insurance providers and plans. Some insurance companies may have an online portal or specific forms to facilitate the preauthorization process, while others may require direct communication between the healthcare provider and the insurance company.
Be sure to follow the instructions provided by your insurance provider and work closely with your healthcare provider to ensure that any necessary preauthorization steps are completed before undergoing STD testing.
Understanding the preauthorization and approval requirements of your insurance plan is crucial to avoid any unexpected denials of coverage or out-of-pocket expenses. Now, let’s discuss the importance of confidentiality and privacy when it comes to STD testing.
Confidentiality and Privacy
Confidentiality and privacy are vital considerations when it comes to STD testing. It is essential for individuals to feel safe and secure when seeking testing and treatment for sexually transmitted infections.
Healthcare providers are bound by strict ethical and legal guidelines to maintain the confidentiality of patient health information, including STD test results. This means that your personal information and test results should be kept private and only shared with authorized individuals on a need-to-know basis.
When you undergo STD testing, your healthcare provider will typically explain the privacy measures in place to protect your information. This can include secure systems for record-keeping, encryption of electronic data, and strict protocols for accessing and sharing sensitive information.
Additionally, many testing facilities and clinics offer anonymous or confidential testing options to further ensure your privacy. These services may allow you to provide limited personal information or use a unique identifier instead of your name. Anonymous testing options may involve using a code or number system, allowing you to receive results without revealing your identity. Confidential testing, on the other hand, means that your personal information is known to the healthcare provider but kept confidential.
Insurance providers also have a responsibility to protect the privacy of your health information. They are bound by federal regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), which safeguards the confidentiality of patient health information. Insurance companies are required to have policies and procedures in place to secure the privacy of your medical records and restrict access to authorized individuals.
It is worth noting that while privacy measures are in place, there may be certain instances where disclosure of health information is required by law. For example, healthcare providers are mandated to report certain communicable diseases, including some STDs, to the appropriate public health authorities.
Ultimately, it is essential to have open and frank discussions with your healthcare provider about confidentiality and privacy concerns. They can clarify the policies and protocols in place to protect your information and address any questions or concerns you may have.
Now that we have covered the importance of confidentiality and privacy, it’s time to wrap up this article.
Conclusion
Navigating the world of STD testing and insurance coverage can be complex, but understanding the key aspects is crucial to being informed and making the best decisions for your health and finances.
Insurance coverage for STD testing varies depending on your specific plan and provider. It’s important to review your policy documents or contact your insurance company to understand the extent of coverage, any cost-sharing responsibilities, and preauthorization requirements.
Types of tests for STDs can range from blood tests to urine tests and swab tests. The costs of these tests can vary, but insurance plans may offer coverage that significantly reduces or eliminates out-of-pocket expenses.
The choice between in-network and out-of-network providers can play a significant role in your insurance coverage. In-network providers often have negotiated rates with your insurance company, resulting in lower costs for you.
Co-payments and deductibles are important financial considerations when it comes to STD testing. Understanding these terms and how they apply to your insurance plan is essential to estimate your out-of-pocket expenses accurately.
Confidentiality and privacy are critical when undergoing STD testing. Healthcare providers and insurance companies are bound by legal and ethical obligations to protect your personal and health information.
By being aware of these crucial aspects and engaging in open communication with your healthcare provider and insurance company, you can navigate the process of STD testing with confidence and ensure that you receive the necessary care while minimizing your financial burden.
Remember, regular STD testing is an essential part of maintaining your sexual health. Early detection and treatment can prevent complications and the spread of infections to others.
Stay informed, prioritize your health, and make the most of your insurance coverage for STD testing. Stay healthy, stay safe!