Finance
What Is A TB Risk Assessment
Published: January 15, 2024
Learn how to assess the financial risk in TB investments and make informed decisions. Understand the key factors impacting finance in TB and mitigate potential risks.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for LiveWell, at no extra cost. Learn more)
Table of Contents
- Introduction
- Definition of TB Risk Assessment
- Purpose of TB Risk Assessment
- Importance of TB Risk Assessment
- Process of TB Risk Assessment
- Elements of TB Risk Assessment
- Tools and Methods for TB Risk Assessment
- Factors Considered in TB Risk Assessment
- Limitations of TB Risk Assessment
- Application of TB Risk Assessment
- Conclusion
Introduction
Welcome to our comprehensive guide on TB risk assessment. Tuberculosis (TB) is a potentially serious infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also impact other parts of the body. TB is highly contagious and can spread from person to person through the air when someone with active TB coughs or sneezes.
Given the serious nature of TB, it is crucial to identify individuals who are at a higher risk of contracting or transmitting the disease. This is where TB risk assessment comes into play. TB risk assessment is a systematic evaluation process used to determine an individual’s likelihood of being exposed to TB or developing active TB disease.
The main purpose of TB risk assessment is to identify individuals who may require further testing, intervention, or preventive measures to reduce the risk of TB transmission and progression. By identifying those at higher risk, healthcare providers can direct resources and interventions more effectively, improving overall TB control measures.
Understanding the importance of TB risk assessment is essential in implementing targeted interventions and preventive strategies. By identifying individuals at risk, health authorities can allocate resources efficiently, improve case detection, and reduce the burden of TB in communities. It is a critical component of TB control programs and helps in designing appropriate prevention and control strategies.
The process of TB risk assessment involves evaluating various factors such as personal and medical history, demographic characteristics, exposure risk, and previously conducted TB tests. By assessing these factors, healthcare professionals can determine the risk level and tailor interventions accordingly. This process helps identify individuals who need further testing, treatment, or preventive therapy.
In the following sections, we will delve deeper into the elements of TB risk assessment, the tools and methods used, the factors considered, the limitations, and the practical application of this assessment process. Understanding these aspects will provide a comprehensive overview of TB risk assessment and its significance in the field of public health.
Definition of TB Risk Assessment
TB risk assessment refers to a systematic evaluation process used to determine the likelihood of an individual being exposed to tuberculosis (TB) or developing active TB disease. This assessment aims to identify individuals who may require further testing, intervention, or preventive measures to reduce the risk of TB transmission and progression.
When conducting a TB risk assessment, healthcare providers evaluate various factors such as an individual’s personal and medical history, demographic characteristics, exposure risk, and previous TB test results. These factors help in determining the level of risk and guiding appropriate interventions.
It is important to note that TB risk assessment is not a diagnostic tool, but rather a screening process. It helps identify individuals who may need further diagnostic tests, such as a TB skin test or a chest X-ray, to confirm the presence of TB infection or disease.
The goal of TB risk assessment is to identify individuals who are at higher risk of TB exposure or progression. By recognizing those at risk, healthcare providers can target interventions more efficiently, ensuring that the appropriate resources and preventive measures are allocated to those who need them the most.
The assessment process typically involves a series of questions or a structured questionnaire that covers various aspects, including demographic information, occupation, medical history, and potential exposure to TB. The responses help healthcare providers gauge the level of risk and guide further actions.
It is important to remember that TB risk assessment should be conducted regularly for individuals who are at an increased risk of TB exposure, such as healthcare workers, individuals with compromised immune systems, and those living or working in settings where TB transmission is more likely to occur.
Overall, TB risk assessment plays a crucial role in identifying individuals who require further evaluation and intervention, such as TB testing or preventive therapy. It enables healthcare providers to prioritize resources and implement targeted measures to prevent the spread of TB and reduce its impact on individuals and communities.
Purpose of TB Risk Assessment
The main purpose of TB risk assessment is to identify individuals who are at higher risk of being exposed to tuberculosis (TB) or developing active TB disease. By identifying those at risk, healthcare providers can direct resources and interventions more effectively, improving overall TB control measures. There are several specific purposes of TB risk assessment:
- Identifying individuals in need of further testing: TB risk assessment helps identify individuals who may require additional diagnostic tests, such as a TB skin test or a chest X-ray, to confirm the presence of TB infection or disease. It ensures that those who need further evaluation receive the appropriate diagnostic procedures.
- Guiding the implementation of preventive measures: By assessing an individual’s risk level, healthcare providers can determine the need for preventive measures, such as TB prophylaxis or vaccination. This helps reduce the risk of TB transmission and the progression from latent TB infection to active TB disease.
- Identifying individuals for active case finding: TB risk assessment helps identify individuals who may have active TB disease but have not yet been diagnosed. This enables healthcare providers to actively search for cases and initiate appropriate treatment, preventing further transmission of the disease.
- Allocating resources effectively: With limited resources, it is important to prioritize interventions and services. TB risk assessment helps in directing resources to individuals who are at higher risk, ensuring that they receive the necessary testing, treatment, and support.
- Monitoring and evaluating TB control programs: By assessing the risk factors associated with TB, healthcare providers can monitor and evaluate the effectiveness of TB control programs. This enables them to make informed decisions, modify interventions if necessary, and improve overall program effectiveness.
By fulfilling these purposes, TB risk assessment plays a vital role in reducing the burden of TB on individuals and communities. It allows for early detection, appropriate treatment, and targeted preventive measures, significantly contributing to TB control efforts.
Importance of TB Risk Assessment
TB risk assessment holds immense importance in the realm of public health and TB control. It plays a crucial role in identifying individuals who are at higher risk of being exposed to tuberculosis (TB) or developing active TB disease. Here are some key reasons why TB risk assessment is so important:
- Early detection and intervention: TB risk assessment helps in early identification of individuals who may be at risk of TB infection or disease. By identifying these individuals, healthcare providers can implement timely interventions, such as diagnostic testing, treatment, or preventive therapy. Early detection and intervention are essential to prevent the progression of TB infection to active disease and reduce the risk of transmission within the community.
- Targeted allocation of resources: TB risk assessment allows for the targeted allocation of limited resources. By identifying individuals at higher risk, healthcare providers can prioritize the allocation of diagnostic tests, medications, and other resources to those who need them the most. This ensures that resources are used efficiently and effectively.
- Prevention of TB transmission: TB risk assessment helps in identifying individuals who may be at risk of transmitting TB to others. By identifying and intervening in these cases, healthcare providers can implement measures to prevent the spread of TB within the community. This includes providing education on infection control measures, ensuring appropriate treatment for infectious individuals, and implementing contact tracing to identify and screen individuals who may have been exposed.
- Improved TB control measures: TB risk assessment plays a vital role in informing and improving TB control strategies and programs. By analyzing the risk factors associated with TB, healthcare providers can better understand the dynamics of transmission and tailor prevention and control measures accordingly. This includes evaluating the impact of interventions, monitoring program effectiveness, and making informed decisions to enhance TB control efforts.
- Reduced burden on healthcare systems: TB risk assessment helps in reducing the burden on healthcare systems by ensuring that resources are directed to individuals who have a higher likelihood of requiring TB testing, treatment, or preventive measures. This targeted approach improves the efficiency of healthcare services, minimizes unnecessary testing and treatment, and allows for better utilization of resources.
In summary, TB risk assessment is of utmost importance in identifying individuals at risk of TB infection or disease, guiding targeted interventions, preventing transmission, and improving overall TB control measures. By implementing effective risk assessment strategies, we can work towards reducing the burden of TB on individuals, communities, and healthcare systems.
Process of TB Risk Assessment
The process of TB risk assessment involves a systematic evaluation of various factors to determine an individual’s likelihood of being exposed to tuberculosis (TB) or developing active TB disease. It typically includes the following steps:
- Gather relevant information: Healthcare providers start by gathering relevant information about the individual, including personal and medical history, demographic characteristics, and potential exposure to TB. This may involve asking questions about occupation, travel history, previous TB tests, and contact with individuals known to have TB.
- Evaluate risk factors: Based on the gathered information, healthcare providers assess the individual’s risk factors associated with TB. These may include factors such as age, occupation (e.g., healthcare worker), residence in or travel to high TB burden areas, close contact with individuals with infectious TB, immunosuppression, and healthcare or correctional facility exposure.
- Determine risk level: Healthcare providers use the evaluated risk factors to determine the individual’s level of risk. This can range from low to high, with individuals at higher risk requiring more thorough evaluation and intervention.
- Recommend further testing: Based on the determined risk level, healthcare providers may recommend further diagnostic tests to confirm TB infection or disease. This can include a TB skin test, interferon-gamma release assay (IGRA), chest X-ray, or other specialized tests based on the individual’s specific circumstances.
- Develop an appropriate management plan: Once the risk level has been determined and diagnostic tests have been conducted, healthcare providers can develop an individualized management plan. This may involve treatment for active TB disease, initiation of preventive therapy for latent TB infection, or continued monitoring and evaluation for individuals at lower risk.
- Provide education and support: Throughout the process, healthcare providers play a vital role in providing education and support to individuals undergoing TB risk assessment. This includes explaining the purpose and significance of the assessment, addressing any concerns or questions, and providing information on preventive measures, treatment options, and available support services.
The process of TB risk assessment is dynamic and may require regular reassessment, particularly for individuals with ongoing exposure risks or changes in their health status. It is essential to follow-up and monitor individuals based on their determined risk level, ensuring appropriate interventions are implemented as needed.
By following this structured process, healthcare providers can effectively assess an individual’s risk of TB, guide appropriate testing and interventions, and contribute to the overall control and prevention of TB within communities.
Elements of TB Risk Assessment
TB risk assessment involves the evaluation of various elements to determine an individual’s likelihood of being exposed to tuberculosis (TB) or developing active TB disease. These elements provide valuable information that helps healthcare providers assess the level of risk and guide appropriate interventions. Here are the key elements of TB risk assessment:
- Personal and medical history: Gathering information about an individual’s personal and medical history is essential in assessing TB risk. This includes factors such as age, gender, underlying medical conditions (such as HIV/AIDS or diabetes), previous TB infection or disease, history of TB exposure or contact with infectious individuals, and any previous TB testing or treatment.
- Demographic characteristics: Demographic factors can also contribute to TB risk. These include living in or traveling to areas with a high prevalence of TB, belonging to certain ethnic or racial groups with increased TB risk, and socioeconomic factors such as poverty and overcrowded living conditions.
- Exposure risk: Evaluating an individual’s exposure risk is crucial for determining TB risk. This includes assessing occupational exposure, such as healthcare workers or individuals working in correctional facilities or homeless shelters. It also involves considering exposure to individuals with infectious TB, either through close contact or being in settings with a high risk of transmission, such as crowded shelters or prisons.
- Immunosuppression: Individuals with weakened immune systems are at a higher risk of TB infection and progression to active disease. Assessing factors such as HIV infection, organ transplantation, use of immunosuppressive medications, and conditions that compromise the immune system helps identify individuals who may be more susceptible to TB infection or reactivation.
- Healthcare or institutional exposure: Healthcare workers and individuals residing in healthcare or institutional settings may have an increased risk of TB exposure due to the close proximity to infectious individuals. Assessing exposure within these settings is crucial in determining an individual’s TB risk.
- Testing and screening results: Previous TB test results, such as a tuberculin skin test (TST) or interferon-gamma release assay (IGRA), can provide valuable information about an individual’s TB infection status. Evaluating these results helps in determining the risk of latent TB infection or active TB disease.
By assessing these elements, healthcare providers gain comprehensive information about an individual’s risk of TB. This information is vital in guiding further diagnostic testing, initiating preventive measures, and designing appropriate management plans for individuals at higher risk.
It is important to note that these elements may vary depending on the specific context, population, and healthcare setting where the TB risk assessment is being conducted. Healthcare providers should consider local guidelines, recommendations, and epidemiological factors to ensure the accuracy and relevance of the assessment.
Tools and Methods for TB Risk Assessment
TB risk assessment involves the use of various tools and methods to systematically evaluate an individual’s likelihood of being exposed to tuberculosis (TB) or developing active TB disease. These tools and methods provide structured approaches that healthcare providers can utilize to assess risk and guide appropriate interventions. Here are some commonly used tools and methods for TB risk assessment:
- Structured questionnaires: Structured questionnaires or surveys are commonly used to collect relevant information from individuals undergoing TB risk assessment. These questionnaires often cover various aspects, including personal and medical history, demographic characteristics, occupational exposure, travel history, and contact with individuals known to have TB. These questionnaires offer a standardized approach to gather comprehensive information for risk assessment.
- Clinical assessment: Healthcare providers perform a thorough clinical assessment by examining an individual’s medical history, conducting a physical examination, and evaluating any symptoms suggestive of TB disease. Clinical assessment helps in identifying potential risk factors and guiding further diagnostic testing or interventions.
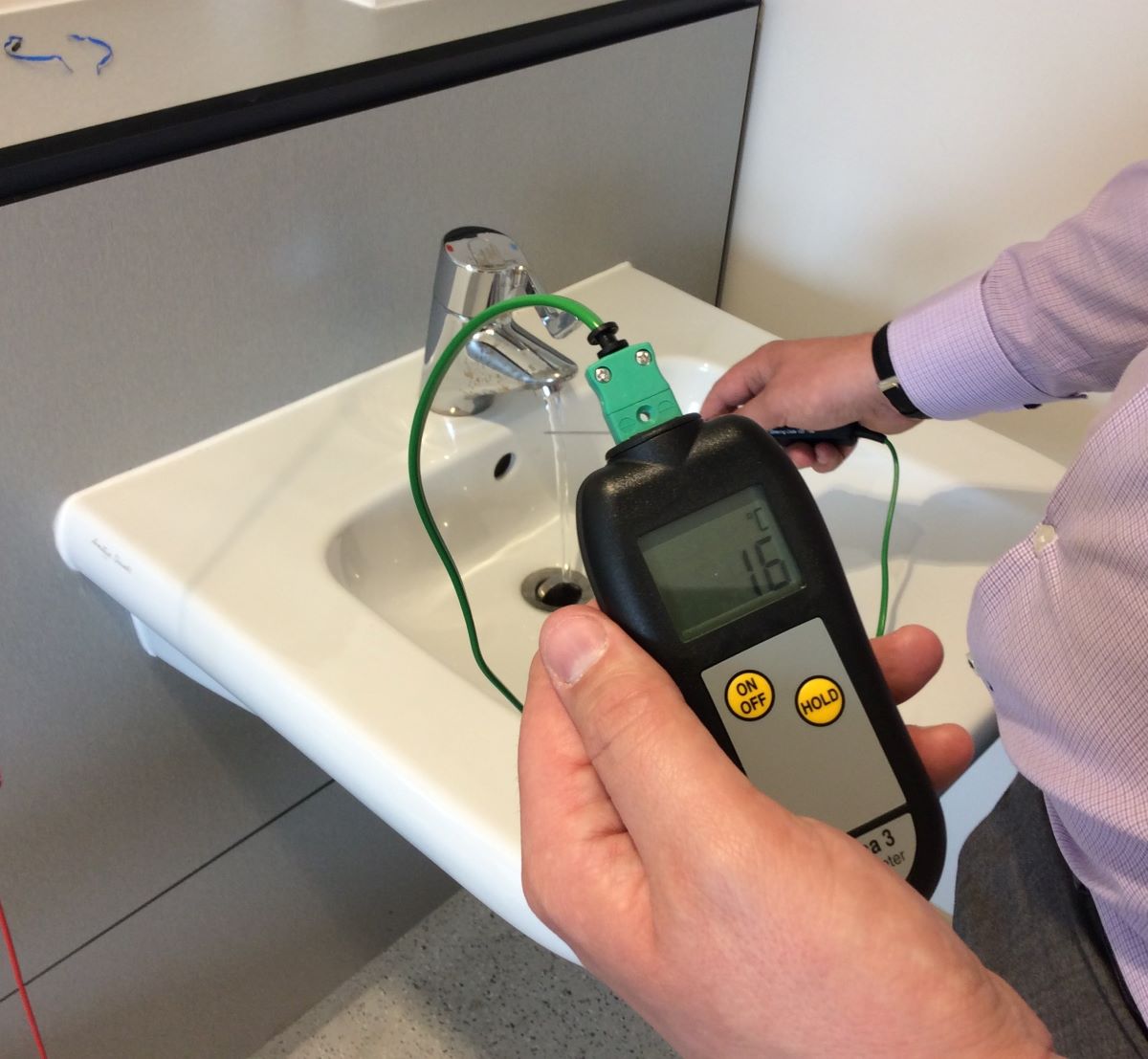
- TB screening tests: TB screening tests, such as tuberculin skin tests (TST) or interferon-gamma release assays (IGRAs), are commonly used to assess an individual’s exposure to TB. These tests detect the presence of TB infection and can help determine latent TB infection or active TB disease.
- Imaging studies: Chest X-rays or other imaging studies are performed to assess the presence of active TB disease in individuals suspected to have TB. These studies help in identifying abnormalities in the lungs, such as TB-related infiltrates or cavities, which are indicative of active TB disease.
- Diagnostic evaluation: In cases where TB infection or disease is suspected based on risk assessment and screening results, additional diagnostic evaluations may be performed. These can include sputum or other specimen collection for smear microscopy, culture, or molecular tests to confirm the presence of TB bacteria.
- Scoring systems: Some healthcare settings or guidelines utilize scoring systems to quantify an individual’s TB risk based on the presence of specific risk factors. These scoring systems assign points to each risk factor and provide a total score that corresponds to the level of risk.
These tools and methods are used in combination to gather information, assess risk factors, and guide appropriate interventions. The selection of specific tools or methods may vary depending on the local guidelines, resources, and the population being assessed. Healthcare providers should adhere to established protocols and guidelines to ensure consistent and accurate TB risk assessment.
It is important to note that these tools and methods are not standalone diagnostic tests for TB; rather, they provide valuable information to aid in the assessment of an individual’s TB risk. Diagnostic tests, such as sputum culture or molecular tests, may be required to confirm the presence of TB infection or disease.
Factors Considered in TB Risk Assessment
When conducting a tuberculosis (TB) risk assessment, healthcare providers take into account various factors to determine an individual’s likelihood of being exposed to TB or developing active TB disease. These factors provide valuable information to assess an individual’s risk level and guide appropriate interventions. Here are the key factors considered in TB risk assessment:
- Personal and medical history: Healthcare providers evaluate an individual’s personal and medical history to identify any factors that may increase the risk of TB. This includes assessing previous TB infection or disease, history of TB exposure or contact with infectious individuals, underlying medical conditions (such as HIV/AIDS or diabetes), and any previous TB testing or treatment.
- Demographic characteristics: Demographic factors play a role in TB risk assessment. Age, gender, race or ethnicity, and socioeconomic status can influence an individual’s risk of TB. Certain population groups, such as individuals from countries with a high TB burden or those living in poverty-stricken areas, may have an increased risk.
- Exposure risk: Evaluating an individual’s exposure risk is crucial in determining the likelihood of TB transmission. Healthcare providers assess occupational exposure, such as healthcare workers or individuals working in correctional facilities or homeless shelters. They also consider exposure to individuals with infectious TB, either through close contact or being in settings with a high risk of transmission, such as crowded living conditions.
- Immunosuppression: Individuals with weakened immune systems are at a higher risk of TB infection and progression to active disease. Factors such as HIV infection, organ transplantation, use of immunosuppressive medications, and other immunocompromising conditions increase the likelihood of developing TB disease.
- Healthcare or institutional exposure: Healthcare workers and individuals residing in healthcare or institutional settings may have an increased risk of TB exposure due to close contact with infectious individuals. Assessing exposure within these settings is important to determine an individual’s risk level.
- Testing and screening results: Previous TB test results, such as tuberculin skin tests (TST) or interferon-gamma release assays (IGRAs), provide valuable information about an individual’s TB infection status. Evaluating these results helps determine the risk of latent TB infection or active TB disease.
These factors are assessed collectively to determine an individual’s level of risk for TB. By considering these factors, healthcare providers can identify individuals who require further evaluation, testing, treatment, or preventive measures. It is important to conduct a thorough assessment of these factors to ensure accurate risk stratification and appropriate interventions for individuals.
It is worth noting that the specific factors considered in TB risk assessment may vary based on local epidemiology, guidelines, and the population being assessed. Healthcare providers should follow established protocols and guidelines to ensure consistent and reliable risk assessment practices.
Limitations of TB Risk Assessment
While TB risk assessment is an important tool in identifying individuals at higher risk of tuberculosis (TB), it is essential to recognize its limitations. Understanding these limitations helps healthcare providers interpret the results of a risk assessment and implement appropriate interventions. Here are some key limitations of TB risk assessment:
- Subjectivity: TB risk assessment relies on the accuracy and completeness of the information provided by the individual. Factors such as recall bias, incomplete information, or reluctance to disclose relevant details may limit the accuracy of the assessment.
- Limited predictive value: TB risk assessment is a screening tool and does not provide definitive diagnostic information. While it helps identify individuals at higher risk, it cannot predict with certainty who will develop active TB disease or when it will occur. It is important to combine risk assessment with appropriate diagnostic tests to confirm TB infection or disease.
- Variable sensitivity and specificity: Different risk factors and scoring systems used in TB risk assessment may have varying sensitivities and specificities. This may result in false positives or false negatives, leading to misclassification of an individual’s TB risk status.
- Dynamic nature of risk factors: Risk factors for TB can change over time. An individual’s risk level may increase or decrease based on changes in demographics, exposure factors, or health status. Static risk assessments may not capture these dynamic changes adequately.
- Geographical and contextual variations: The risk factors associated with TB can vary across different geographical regions and populations. Factors such as TB prevalence, transmission dynamics, and healthcare resources can influence the relevance and applicability of specific risk factors in different settings.
- Underlying social determinants of TB: TB risk assessment often focuses on individual-level risk factors. However, TB transmission and susceptibility are also influenced by broader social determinants, such as poverty, homelessness, and access to healthcare. These social factors may not be fully captured in the assessment process.
- Potential for stigma and discrimination: The process of TB risk assessment may inadvertently lead to stigma and discrimination, particularly if individuals are labeled as being at high risk. It is important to approach risk assessment sensitively and ensure that individuals are provided with appropriate support, education, and privacy protections.
Despite these limitations, TB risk assessment remains a valuable tool for identifying individuals who may require further evaluation and interventions for TB. It helps guide targeted interventions, resource allocation, and preventive measures. By recognizing the limitations and addressing them appropriately, healthcare providers can maximize the benefits of TB risk assessment in TB control efforts.
Application of TB Risk Assessment
TB risk assessment has several important applications in the field of tuberculosis (TB) control and prevention. It plays a crucial role in identifying individuals who require further evaluation, testing, treatment, or preventive measures. Here are some key applications of TB risk assessment:
- Infection control measures: TB risk assessment helps identify individuals who may pose a higher risk of TB transmission. This allows healthcare facilities to implement appropriate infection control measures, such as respiratory precautions and isolation, to prevent the spread of TB within healthcare settings.
- Targeted testing and treatment: Based on the results of TB risk assessment, healthcare providers can prioritize individuals for TB testing, including tuberculin skin tests (TST) or interferon-gamma release assays (IGRAs). This helps in the early detection of TB infection and disease, ensuring prompt treatment initiation and reducing the risk of transmission.
- Preventive therapy: TB risk assessment is instrumental in identifying individuals who are at risk of developing active TB disease from latent TB infection. With risk assessment, healthcare providers can determine the eligibility for and initiate appropriate preventive therapy, such as the use of isoniazid for latent TB infection. This helps in reducing the risk of disease progression.
- Contact tracing: TB risk assessment assists in identifying individuals who have been in close contact with individuals diagnosed with infectious TB. This allows for the implementation of contact tracing efforts, which involve screening and testing individuals who may have been exposed to TB. Early identification and treatment of TB infection in contacts help prevent the development of active TB disease.
- Occupational health: TB risk assessment is particularly relevant in occupational health settings, such as healthcare facilities. It helps identify healthcare workers who may have an increased risk of TB due to their work environment. By implementing appropriate preventive measures and regular screening, the risk of TB transmission within healthcare settings can be minimized.
- Program planning and resource allocation: TB risk assessment provides valuable information on the population-level distribution of TB risks. This helps public health officials and policymakers in planning targeted interventions, allocating resources effectively, and prioritizing high-risk individuals or communities in TB control programs.
By applying TB risk assessment in these various ways, healthcare providers, public health officials, and policymakers can enhance TB control efforts. It ensures that preventive and treatment measures are targeted towards those individuals who are at higher risk, leading to more efficient resource utilization, decreased transmission rates, and improved patient outcomes.
Conclusion
TB risk assessment is a crucial tool in identifying individuals who are at higher risk of being exposed to tuberculosis (TB) or developing active TB disease. By evaluating various factors such as personal and medical history, demographic characteristics, exposure risk, and previous TB test results, healthcare providers can determine the level of risk and guide appropriate interventions.
The importance of TB risk assessment lies in its ability to facilitate early detection, targeted interventions, and resource allocation. By identifying high-risk individuals, healthcare providers can prioritize testing, treatment, and preventive measures, ultimately reducing the burden of TB on individuals and communities.
However, it is essential to acknowledge the limitations of TB risk assessment. Factors such as subjectivity, limited predictive value, and variable sensitivity and specificity can impact the accuracy and reliability of the assessment. Additionally, the dynamic nature of risk factors and contextual variations should be considered when interpreting the results of a risk assessment.
Despite these limitations, TB risk assessment finds practical application in various areas. It helps in implementing infection control measures, guiding testing and treatment decisions, initiating preventive therapy for latent TB infection, conducting contact tracing efforts, addressing occupational health risks, and informing program planning and resource allocation.
In conclusion, TB risk assessment is a valuable tool in the fight against TB. It enables healthcare providers, public health officials, and policymakers to identify individuals who are at higher risk, implement appropriate interventions, and allocate resources efficiently. By integrating TB risk assessment into comprehensive TB control strategies, we can work towards reducing the incidence and impact of TB, promoting early detection, and improving the health outcomes of individuals and communities affected by this global health concern.