Finance
What Is Cash Flow In A Medical Practice?
Published: December 21, 2023
Learn about the importance of cash flow in a medical practice and how it impacts the financial health. Discover key finance strategies to optimize cash flow and boost profitability.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for LiveWell, at no extra cost. Learn more)
Table of Contents
Introduction
Running a successful medical practice requires a careful balance of providing quality patient care, managing expenses, and ensuring a steady flow of revenue. One critical aspect of managing a medical practice’s financial health is cash flow. Cash flow refers to the movement of money into and out of a business, and it is vital for the day-to-day operations and long-term sustainability of a medical practice.
In simple terms, cash flow is the amount of money that is available to a medical practice at any given time. It is not just about how much revenue a practice generates; it is also about when that revenue is received and how it is managed. Cash flow management involves monitoring the inflow and outflow of funds to ensure there is sufficient liquidity to cover expenses, pay staff, invest in equipment and technology, and generate a profit.
Proper cash flow management is crucial for a medical practice for several reasons. First and foremost, it ensures that the practice has the financial resources to cover its day-to-day operational expenses. These expenses include rent, utilities, staff salaries, medical supplies, and other overhead costs. Without adequate cash flow, a medical practice may struggle to meet these financial obligations, leading to disruptions in patient care and potentially damaging the practice’s reputation.
Moreover, an efficiently managed cash flow allows a medical practice to take advantage of growth opportunities. Whether it’s expanding services, hiring additional staff, or investing in new technologies, these endeavors require capital. By maintaining positive cash flow and having a reserve of funds, a practice can pursue these growth initiatives and ultimately enhance its competitiveness and profitability.
On the other hand, poor cash flow management can have severe consequences for a medical practice. It can lead to delays in paying suppliers and vendors, resulting in strained relationships. It can also make it challenging to attract and retain top talent if there are uncertainties around payroll. Additionally, inadequate cash flow can hinder a practice’s ability to invest in necessary equipment and technology, impairing its ability to deliver quality patient care.
Given the critical role that cash flow plays in the success of a medical practice, it is crucial for healthcare professionals to understand the factors that affect cash flow, implement effective strategies for managing it, and address common cash flow issues. By doing so, medical practices can optimize financial stability, maintain a healthy bottom line, and provide excellent care to their patients.
Definition of Cash Flow
Cash flow, in the context of a medical practice, refers to the movement of money into and out of the business over a specific period of time. It represents the net amount of cash generated or used by the practice to meet its financial obligations and fund its operations.
There are three primary components of cash flow:
- Inflows: Inflows represent the sources of cash coming into the medical practice. This includes payments from patients, insurance reimbursements, government incentives, and any other revenue generated by the practice. Proper management of inflows involves ensuring timely and accurate billing, efficient claims processing, and effective patient collections.
- Outflows: Outflows refer to the cash that flows out of the medical practice to cover expenses. This includes operational expenses such as rent, utilities, staff salaries, medical supplies, and equipment costs. It also includes payments to vendors, loan repayments, and any other financial obligations of the practice. Managing outflows involves budgeting, expense control, and negotiating favorable terms with suppliers and lenders.
- Net Cash Flow: Net cash flow is calculated by subtracting the total outflows from the total inflows. A positive net cash flow indicates that the practice is generating more cash than it is spending, which is generally considered favorable. Conversely, a negative net cash flow means that the practice is spending more cash than it is receiving, which could indicate financial challenges or inefficiencies in cash flow management.
It is important to note that cash flow is different from profitability. Profitability is a measure of how much money a medical practice is making after accounting for all costs and expenses. Cash flow, on the other hand, focuses solely on the movement of money in and out of the practice without considering non-cash items such as depreciation or accruals.
There are two main types of cash flow:
- Operating Cash Flow: Operating cash flow relates to the cash generated or used by the core operations of the medical practice. It takes into account the revenue from patient services, the cost of providing those services, and other operational expenses. Operating cash flow is a key measure of the practice’s ability to generate sufficient cash from its day-to-day operations.
- Investing and Financing Cash Flow: Investing cash flow reflects any cash inflows or outflows related to investments in property, plant, and equipment, as well as any financing activities such as obtaining loans or issuing equity. These activities impact the practice’s overall cash position and its ability to invest in growth opportunities.
By understanding the different components and types of cash flow, medical practices can better manage their financial resources, optimize revenue generation, and ensure the long-term stability and success of the practice.
Importance of Cash Flow in a Medical Practice
Cash flow is a critical aspect of managing a medical practice’s financial health. It plays a significant role in ensuring the smooth operation and long-term sustainability of the practice. Here are some key reasons why cash flow is important:
- Working Capital Management: Cash flow is essential for maintaining adequate working capital in a medical practice. Working capital is the difference between current assets (cash, accounts receivable, inventory) and current liabilities (accounts payable, accrued expenses). Sufficient working capital allows the practice to cover day-to-day operational expenses, such as staff salaries, rent, utilities, and medical supplies, without relying on external funding sources. Effective cash flow management helps to avoid cash shortages and ensures the practice can meet its financial obligations in a timely manner.
- Patient Care and Service: Cash flow directly impacts a medical practice’s ability to provide quality patient care and service. It ensures that the practice has the necessary funds to invest in state-of-the-art medical equipment and technology, hire skilled healthcare professionals, and maintain a comfortable and efficient facility. A positive cash flow enables the practice to deliver optimal patient care, attract and retain patients, and establish a reputable brand in the healthcare industry.
- Expense Management: Effective cash flow management helps a medical practice control its expenses. By monitoring cash inflows and outflows, the practice can identify areas where expenses can be reduced or eliminated, optimizing operational efficiency. Proper expense management not only contributes to a positive cash flow but also improves the practice’s profitability and financial stability.
- Investment Opportunities: Maintaining a healthy cash flow positions a medical practice to seize growth and investment opportunities. Whether it’s expanding services, opening additional locations, or implementing new technologies, these endeavors require capital. With positive cash flow, the practice can allocate funds towards growth initiatives, enhancing its competitive edge and potential for increased revenue and profitability.
- Reduced Financing Costs: A medical practice with a positive cash flow is less reliant on external financing options, such as loans or lines of credit, to cover operational expenses or invest in growth. By reducing the need for external financing, the practice can minimize interest costs and maintain greater financial independence.
- Emergency Situations: Cash flow is crucial for managing unexpected events or emergencies that may arise in a medical practice. Having a reserve of cash ensures that the practice can navigate through unforeseen challenges, such as equipment breakdowns, natural disasters, or sudden changes in reimbursements.
In summary, cash flow is vital in a medical practice as it enables the practice to effectively manage working capital, provide quality patient care, control expenses, pursue growth opportunities, reduce financing costs, and have financial resilience during emergencies. By maintaining a healthy cash flow, medical practices can achieve long-term financial stability and success.
Factors Affecting Cash Flow in a Medical Practice
A variety of factors can impact the cash flow of a medical practice. Understanding these factors is crucial for effectively managing cash flow and ensuring financial stability. Here are some key factors that can influence cash flow in a medical practice:
- Reimbursement and Billing: The timely and accurate processing of insurance claims and patient billing is crucial for cash flow. Delays in reimbursements from insurance companies can lead to cash flow gaps, while errors in billing can result in payment discrepancies and longer collection cycles. Ensuring efficient and effective billing processes, including proper coding and submission of claims, can help accelerate cash inflows and reduce payment delays.
- Patient Collections: Collecting payments from patients in a timely manner is essential for maintaining a healthy cash flow. High deductibles, copayments, and outstanding patient balances can create challenges in cash collection. Implementing clear and transparent payment policies, leveraging technology for electronic payments, and proactively communicating with patients about their financial responsibilities can help improve patient collections and cash flow.
- Seasonality and Patient Flow: Some medical practices may experience variations in patient volume and revenue due to seasonal fluctuations or other external factors. For example, a dermatology practice may have higher patient demand during the summer months. Understanding the seasonality patterns in the practice’s specialty and planning accordingly can help manage cash flow during periods of lower patient flow.
- Operational Expenses: The management of operational expenses is crucial for cash flow. Monitoring and controlling expenses such as rent, staff salaries, medical supplies, and utilities can help maintain a positive cash flow. Negotiating favorable terms with vendors, implementing cost-saving measures, and regularly reviewing and adjusting the practice’s budget can contribute to efficient expense management and improved cash flow.
- Insurance Contracts: The terms and conditions of insurance contracts can impact the timing and amount of reimbursements received by a medical practice. Contractual adjustments, negotiated rates, and varying reimbursement schedules can influence cash flow. Understanding the intricacies of insurance contracts, regularly reviewing contract terms, and negotiating favorable agreements can help optimize reimbursements and cash flow.
- Bad Debt and Uncollectible Accounts: Managing bad debt and uncollectible accounts is essential for maintaining cash flow. Unpaid patient balances, delinquent accounts, and non-payment by insurance companies can adversely impact cash flow. Implementing robust financial policies, effective collection processes, and utilizing technology for tracking and reducing bad debt can help minimize cash flow disruptions.
- Payer Mix: The mix of payers can also affect cash flow in a medical practice. Practices heavily reliant on government payers, such as Medicaid or Medicare, may experience delayed reimbursements or lower reimbursement rates. Diversifying the payer mix and actively seeking contracts with commercial insurance companies can help mitigate potential cash flow challenges.
- Growth and Expansion: While growth and expansion can bring opportunities, they can also strain cash flow. Investing in new equipment, hiring additional staff, and opening new locations require upfront capital. Proper financial planning and securing adequate funding sources are crucial to support growth initiatives without negatively impacting cash flow.
By considering and addressing these factors, medical practices can proactively manage their cash flow, optimize revenue generation, and maintain financial stability.
Strategies for Managing Cash Flow
Effectively managing cash flow is essential for the financial health and stability of a medical practice. Here are some strategies to help medical practices better manage their cash flow:
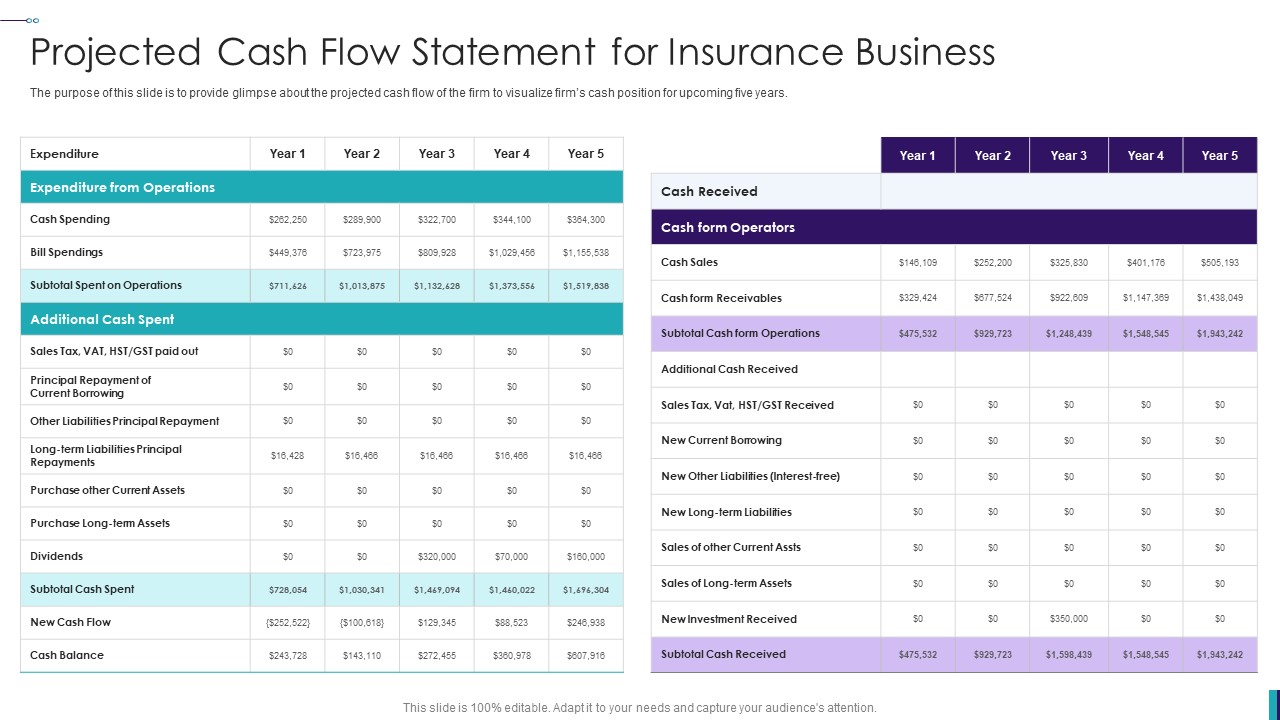
- Create a Cash Flow Forecast: Developing a cash flow forecast allows the practice to anticipate and plan for future cash inflows and outflows. It provides visibility into expected revenue, expenses, and potential cash shortfalls. By regularly reviewing and updating the cash flow forecast, the practice can proactively identify and address potential cash flow challenges.
- Monitor and Accelerate Inflows: Actively managing and accelerating cash inflows is crucial for cash flow management. Implement efficient billing processes, ensuring accurate and timely submission of claims, and optimized reimbursement processes. Explore options for electronic payment methods and provide clear payment terms to encourage prompt payments from patients.
- Negotiate Payment Terms with Vendors: Negotiating favorable payment terms with vendors can help improve cash flow. Extend payment terms where possible to align with revenue cycles and cash inflows. Consider negotiating discounts for early payment and build strong relationships with key suppliers to secure better terms.
- Optimize Operating Expenses: Regularly review expenses and identify areas where costs can be reduced without compromising patient care. Explore opportunities for bulk purchasing of supplies, negotiate lower rates with service providers, and find ways to increase operational efficiency.
- Improve Patient Collections: Implement clear and transparent payment policies and provide multiple payment options to make it easier for patients to pay their bills. Regularly communicate with patients about their financial obligations, educate them about insurance coverage and copayments, and offer payment plans for larger balances.
- Manage Debt and Credit: Minimize borrowing costs by managing debt and credit effectively. Regularly review and renegotiate loan terms, consolidate debts where possible, and maintain a good relationship with financial institutions. Avoid unnecessary borrowing and consider alternative financing options when needed.
- Establish Cash Flow Reserves: Building up a cash reserve helps cushion the practice against unexpected events or emergencies. Set aside a portion of the revenue to create a cash reserve that can cover expenses during periods of reduced cash flow or unforeseen circumstances.
- Regularly Review and Update Financial Policies: Review financial policies and procedures regularly to ensure they are current, effective, and aligned with the practice’s goals. Stay informed about industry trends, regulatory changes, and reimbursement updates to ensure financial policies are adapted accordingly.
- Utilize Technology: Leverage technology to streamline billing processes, automate payment collection, and improve overall financial management. Adopt electronic health record (EHR) systems with integrated billing capabilities, implement online payment portals, and use financial management software to track and monitor cash flow.
- Consult with Financial Professionals: Seek advice from financial professionals, such as accountants or healthcare consultants, to gain insights and expertise in cash flow management. They can provide guidance on financial strategies, offer recommendations for improving cash flow, and help identify areas for financial optimization.
By implementing these strategies, medical practices can improve their cash flow management, maintain financial stability, and ensure a steady income stream to support the delivery of quality patient care.
Common Cash Flow Issues in Medical Practices
While cash flow management is crucial for the financial health of a medical practice, various common issues can disrupt the cash flow cycle. It is important to identify and address these challenges proactively to maintain a healthy cash flow. Here are some common cash flow issues that medical practices may encounter:
- Delayed Insurance Reimbursements: Delays in receiving insurance reimbursements can significantly impact cash flow. Submitting claims accurately and promptly, following up on claim status, and maintaining open lines of communication with insurance companies can help minimize delays and ensure timely payments.
- High Rate of Accounts Receivable: A high volume of outstanding accounts receivable can restrict cash flow. Implementing effective patient collections strategies, such as clear payment policies and timely follow-up on unpaid balances, can help reduce the accounts receivable backlog and improve cash flow.
- Seasonal Fluctuations: Some medical practices may experience seasonal fluctuations in patient volume, resulting in variations in cash flow. Understanding and planning for these fluctuations, such as adjusting staff schedules or implementing marketing strategies to attract patients during slower periods, can help mitigate the impact on cash flow.
- Overdue Accounts Payable: Delayed payments to vendors and suppliers can strain cash flow and strain relationships. Monitoring accounts payable, negotiating extended payment terms when appropriate, and ensuring timely payment of invoices can help maintain positive vendor relationships and avoid disruptions in supplies and services.
- Insufficient Financial Reserves: Lack of sufficient cash reserves can make it challenging to manage cash flow during unexpected events or emergencies. Creating and maintaining a financial reserve to handle unforeseen circumstances can provide a buffer and help ensure a steady cash flow during difficult periods.
- Poor Expense Management: Inefficient expense management can result in excessive spending and impact cash flow. Regularly reviewing expenses, seeking cost-saving opportunities, and implementing budgetary controls can help optimize expenses and preserve cash flow.
- Inadequate Billing and Coding Processes: Errors in billing and coding can lead to payment delays and denials, negatively affecting cash flow. Implementing robust billing and coding processes, training staff on best practices, and utilizing technology for accurate and timely submissions can help minimize billing issues and improve cash flow.
- Limited Access to Capital: Limited access to capital can hinder cash flow management, especially during periods of growth or when additional investments are required. Exploring financing options, establishing relationships with lenders, and maintaining a good credit history can increase access to capital when needed and support cash flow management.
- Inefficient Revenue Cycle Management: Inefficient revenue cycle management, including delays in claim processing or lack of follow-up on unpaid claims, can impact cash flow. Implementing efficient revenue cycle workflows, utilizing technology for automated claims processing and denials management, and regularly monitoring key metrics can help improve revenue cycle efficiency and cash flow.
- Inaccurate Financial Forecasting: Inaccurate financial forecasting can lead to cash flow surprises and inadequate planning. Regularly reviewing and updating financial forecasts, considering various scenarios, and seeking professional guidance can help improve the accuracy of financial projections and aid in better cash flow management.
By being aware of these common cash flow issues and taking proactive measures to address them, medical practices can maintain a steady cash flow, optimize revenue generation, and ensure long-term financial stability.
Tips for Improving Cash Flow in a Medical Practice
A strong cash flow is crucial for the financial success and sustainability of a medical practice. Here are some tips to help improve cash flow and ensure the smooth operation of the practice:
- Streamline Billing Processes: Implement efficient billing processes to ensure accurate and timely claim submissions. Verify patient insurance coverage, verify demographic information, and use technology to automate and streamline the billing workflow. This will help accelerate reimbursement and minimize payment delays.
- Optimize Revenue Cycle Management: Focus on optimizing the revenue cycle by closely monitoring key performance indicators (KPIs). Track claim denials, average days in accounts receivable, and collections rate. Identify bottlenecks and implement strategies to minimize denials and shorten the revenue cycle, leading to improved cash flow.
- Strengthen Patient Collections: Proactively communicate with patients about their financial responsibility, providing clear explanations of insurance coverage and payment obligations. Implement electronic payment options, offer convenient payment plans, and follow up on outstanding balances to improve patient collections and cash flow.
- Negotiate Favorable Payment Terms: Establish relationships with vendors and suppliers and negotiate favorable payment terms. Request extended payment periods or explore discounts for early payment. By negotiating better terms, the practice can manage cash flow more effectively and optimize cash reserves.
- Control Operating Expenses: Regularly review and analyze operating expenses to identify areas for cost reduction. Negotiate contracts with suppliers to obtain lower rates, explore group purchasing organizations (GPOs) for cost savings, and implement efficient inventory management practices to control supply costs.
- Diversify Payer Mix: Reduce reliance on one or two payers by diversifying the practice’s payer mix. This can help mitigate the impact of changes in reimbursement rates or delays in payments. Actively seek contracts with commercial insurance companies to broaden the practice’s revenue sources.
- Implement Financial Policies: Develop and enforce clear financial policies that cover patient payment expectations, collections procedures, and insurance verification processes. Make sure patients understand their financial obligations upfront, minimizing the risk of unpaid balances and improving cash flow.
- Invest in Technology: Leverage technology to streamline processes and improve efficiency. Implement electronic health record (EHR) systems with integrated billing capabilities, automate appointment reminders and patient communications, and utilize financial management software for accurate tracking of cash flow and expenses.
- Establish a Cash Reserve: Build up a cash reserve to serve as a buffer for unexpected events or emergencies. Set aside a portion of revenue each month to create a reserve that can cover expenses during periods of reduced cash flow. This ensures the practice can still function smoothly even during challenging times.
- Seek Professional Guidance: Consult with financial professionals, such as accountants or healthcare consultants, to gain expertise in cash flow management. They can provide insights into financial strategies, help with financial forecasting, and offer guidance on improving cash flow and overall financial health.
By implementing these tips and adopting a proactive approach to cash flow management, medical practices can optimize revenue, minimize payment delays, control expenses, and ensure a healthy and sustainable financial future.
Conclusion
Cash flow is a fundamental aspect of managing a successful medical practice. It plays a vital role in maintaining the practice’s financial stability, supporting quality patient care, and enabling growth opportunities. Understanding the factors that affect cash flow and implementing effective strategies for cash flow management are essential for the long-term success of a medical practice.
By maintaining a positive cash flow, medical practices can ensure there are sufficient funds to cover day-to-day operational expenses, invest in necessary equipment and technology, and provide excellent patient care. Timely and accurate billing processes, effective patient collections strategies, and negotiation of favorable payment terms with vendors are critical to improving cash flow.
Additionally, it is crucial to address common cash flow issues such as delayed insurance reimbursements, high accounts receivable, and inefficient revenue cycle management. Optimizing expense management, diversifying payer mix, implementing financial policies, utilizing technology, and establishing a cash reserve can further enhance cash flow and financial stability in a medical practice.
Ultimately, effective cash flow management empowers medical practices to navigate through challenges and seize growth opportunities. It allows them to focus on what matters most – delivering exceptional patient care while maintaining a financially sound and sustainable practice.
To thrive in today’s healthcare landscape, medical practices must prioritize cash flow management as an integral part of their overall financial strategy. By implementing the tips and strategies outlined in this article, medical practices can achieve financial success, improve patient care, and ensure a bright future in an ever-evolving healthcare industry.