Finance
When Would A Biller Bill Secondary Insurance?
Published: November 6, 2023
Learn the finance strategy of when a biller would bill secondary insurance, ensuring proper reimbursement and maximizing financial benefits.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for LiveWell, at no extra cost. Learn more)
Table of Contents
Introduction
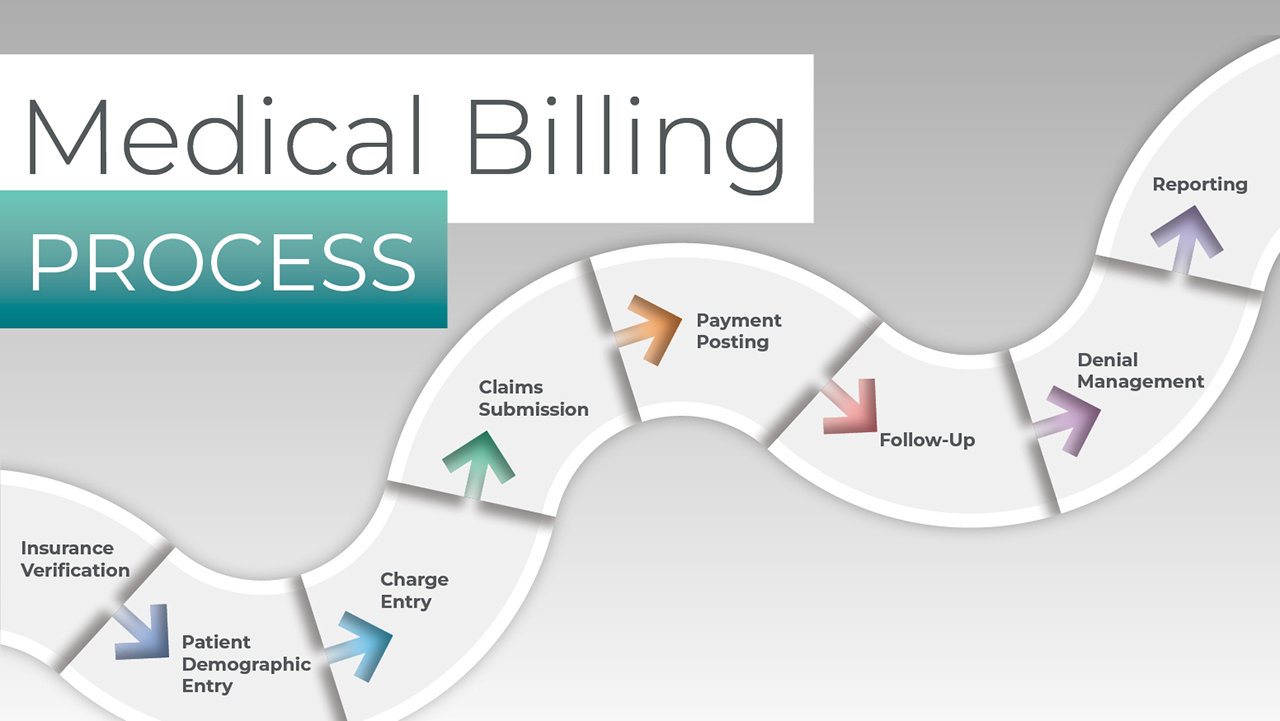
In the world of insurance, individuals often have multiple policies to cover their healthcare expenses. This is known as primary and secondary insurance. Understanding how primary and secondary insurance work together is crucial for healthcare providers and billers to ensure efficient reimbursement processes. Knowing when to bill secondary insurance can significantly impact the revenue cycle and prevent costly errors.
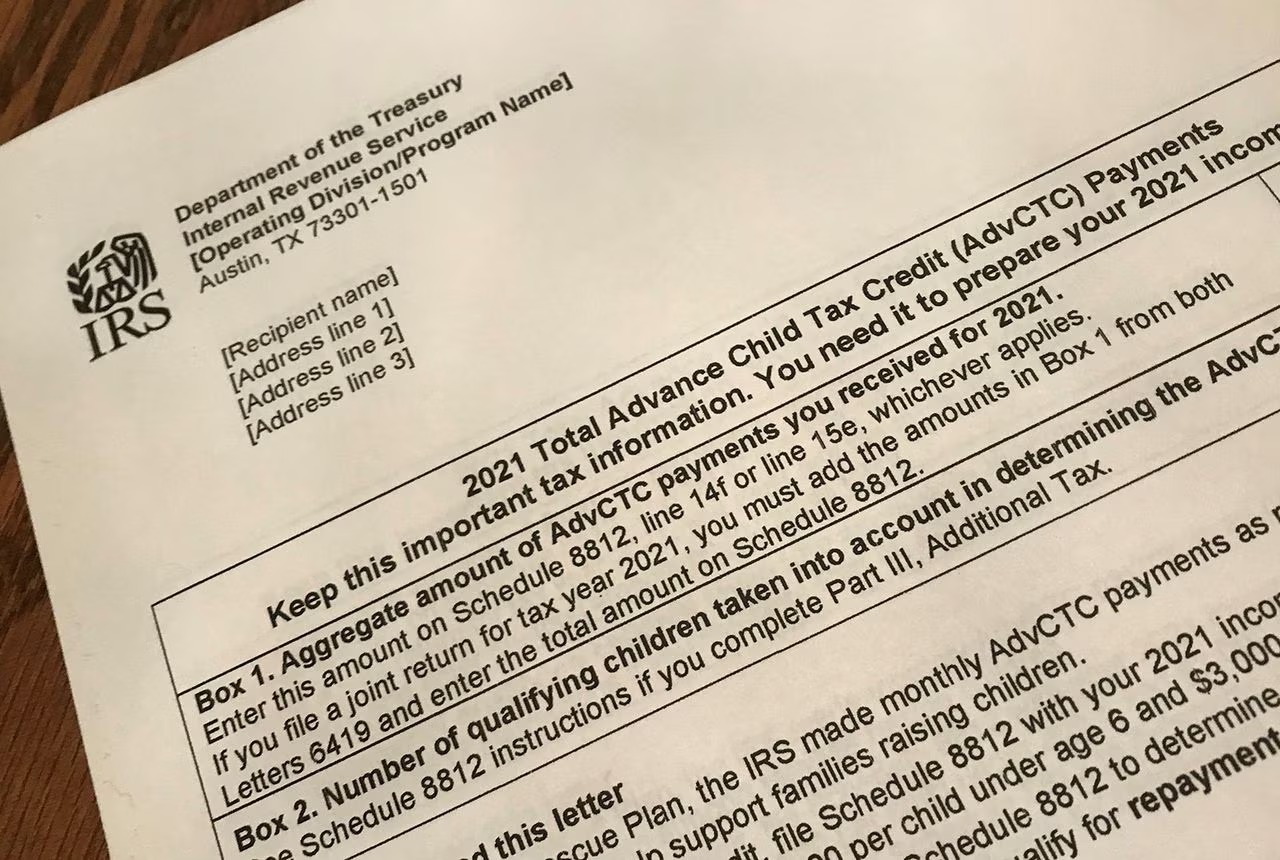
Primary insurance is the first policy that covers medical expenses. It could be the insurance plan held by the individual themselves, through an employer, or through a government program like Medicare or Medicaid. Secondary insurance, on the other hand, is an additional policy that can be used to cover any remaining expenses not covered by the primary insurance.
The question then arises, when should a biller bill secondary insurance? There are several scenarios in which it becomes necessary to bill secondary insurance for proper reimbursement. These scenarios include deductibles and co-payments, coverage gaps, and coordination of benefits.
In this article, we will explore these scenarios in detail and provide insights into when billers should consider billing secondary insurance, ensuring proper reimbursement and minimizing financial burden on patients.
Understanding Primary and Secondary Insurance
Before diving into when to bill secondary insurance, it’s essential to have a clear understanding of primary and secondary insurance and how they work together.
Primary insurance is the first line of coverage that individuals have for their healthcare expenses. It is the initial policy that pays for medical services. This can be an insurance plan that an individual holds through their employer, a government program like Medicare or Medicaid, or a private insurance policy purchased independently.
Secondary insurance, on the other hand, is an additional policy that individuals may have to cover any remaining expenses that are not covered by the primary insurance. It acts as a safety net to cover the gaps left by the primary insurance policy.
When a person seeks medical treatment, the primary insurance is billed first. It covers the portion of the medical expenses according to the policy’s terms and conditions. Once the primary insurance has paid its share, any remaining balance can be billed to the secondary insurance.
Secondary insurance aims to minimize out-of-pocket expenses for patients. It can step in and cover deductibles, co-payments, and any other expenses not covered by the primary insurance. However, it’s important to note that secondary insurance cannot pay more than the total cost of the medical service.
In some cases, individuals may have multiple secondary insurance policies, depending on their coverage and needs. Each secondary insurance policy functions in the same way, covering the remaining balance beyond what the primary insurance covers.
Understanding the interplay between primary and secondary insurance is crucial for healthcare providers and billers. It ensures that the right insurance policies are billed for proper reimbursement and prevents any financial burdens on the patients.
When to Bill Secondary Insurance
Knowing when to bill secondary insurance is essential for healthcare providers and billers to maximize reimbursement and minimize patient out-of-pocket costs. There are several scenarios in which billers should consider submitting claims to secondary insurance.
Scenario 1: Deductibles and Co-Payments
One common situation that calls for billing secondary insurance is when there are deductible and co-payment obligations. A primary insurance policy may have a deductible requirement, which is the amount that the insured individual must pay out of pocket before the insurance coverage kicks in. If the patient has a secondary insurance policy, the biller should bill the secondary insurance for the deductible amount.
Similarly, co-payments are fixed fees that individuals are required to pay for specific medical services or treatments. If the primary insurance policy requires co-payments, billers should submit the claim to the secondary insurance to cover the remaining co-payment amount after the primary insurance has paid.
Scenario 2: Coverage Gaps
Another instance when billers should bill secondary insurance is when there are coverage gaps in the primary insurance policy. Occasionally, primary insurance plans may exclude certain services or have limitations on coverage. In such cases, the secondary insurance may cover the gaps left by the primary insurance. Billers should carefully review the primary insurance explanation of benefits (EOB) to identify any services that are not covered or have limited coverage. These uncovered or partially covered services can then be billed to the secondary insurance for potential reimbursement.
Scenario 3: Coordination of Benefits
Coordination of benefits (COB) is a critical factor in determining when to bill secondary insurance. COB refers to the process of determining how multiple insurance plans will work together to cover medical expenses. It ensures that the combined payment from primary and secondary insurance does not exceed the total cost of the medical service.
If an individual has both primary and secondary insurance, the biller must determine which insurance is responsible for covering the services first. Generally, the primary insurance is billed first, and any remaining balance can then be billed to the secondary insurance. However, this process may vary depending on the specific coordination of benefits rules and guidelines outlined by the insurance companies.
In some cases, the secondary insurance may require that the primary insurance submit the claim first before they process the claim. In this scenario, the biller should bill the primary insurance and, once the primary insurance has paid, submit the remaining balance to the secondary insurance.
In other cases, the secondary insurance may have a “non-duplication of benefits” policy, which means they will only pay out if the primary insurance’s payment is less than what they would have paid if they were the primary insurance. In these instances, it’s important for billers to coordinate with both the primary and secondary insurance companies to ensure proper billing and reimbursement.
Overall, proper understanding of deductibles, co-payments, coverage gaps, and coordination of benefits is vital for billers to determine when to bill secondary insurance. By accurately identifying these scenarios, billers can ensure that all eligible insurance coverage is utilized, maximizing reimbursement and minimizing financial burdens on patients.
Scenario 1: Deductibles and Co-Payments
One common situation that calls for billing secondary insurance is when there are deductible and co-payment obligations. Both primary and secondary insurance policies may have deductible and co-payment requirements that individuals must fulfill.
A deductible is the amount that the insured individual must pay out of pocket before the insurance coverage kicks in. It is a fixed annual amount that varies depending on the insurance policy. If the patient has a secondary insurance policy, the biller should bill the secondary insurance for the deductible amount.
For example, suppose a patient has a primary insurance policy with a $1,000 deductible and seeks medical treatment. Once the primary insurance processes the claim and applies the deductible, the patient is responsible for paying the deductible amount. However, if the patient also has secondary insurance, the biller should bill the secondary insurance for the deductible amount to minimize the patient’s financial burden.
Co-payments, on the other hand, are fixed fees that individuals are required to pay for specific medical services or treatments. These fees are predetermined by the insurance policy and may vary depending on the type of service or treatment received.
When billing co-payments, the primary insurance may cover a portion of the co-payment, and the patient is responsible for the remaining balance. In this scenario, the biller should submit the claim to the secondary insurance to cover the remaining co-payment amount after the primary insurance has paid.
For example, let’s say a patient undergoes a medical procedure that has a $200 co-payment. The primary insurance policy covers 80% of the co-payment, leaving the patient responsible for the remaining 20%. In this case, the biller can submit the claim to the secondary insurance to cover the outstanding 20% co-payment, reducing the patient’s out-of-pocket costs.
By correctly identifying deductibles and co-payments, billers ensure that both primary and secondary insurance policies are utilized to their full potential. This not only reduces the financial burden on patients but also maximizes reimbursement for healthcare providers.
Scenario 2: Coverage Gaps
Another scenario in which billing secondary insurance becomes necessary is when there are coverage gaps in the primary insurance policy. Despite the comprehensive coverage provided by most primary insurance plans, there may still be certain services or treatments that are not covered or have limited coverage.
When a patient requires a service or treatment that is not covered by their primary insurance policy, the biller should consider billing the secondary insurance to bridge the coverage gap. This ensures that the patient receives necessary healthcare services without incurring excessive out-of-pocket costs.
For example, let’s say a patient needs a specialized therapy for a particular medical condition, but their primary insurance policy does not cover this therapy. In this case, the biller should review the primary insurance explanation of benefits (EOB) to confirm that the therapy is indeed not covered. Then, they can bill the secondary insurance to explore if the therapy is covered under that policy.
In some instances, the primary insurance policy may cover the treatment partially, leaving the patient responsible for a significant portion of the expenses. In such cases, the secondary insurance can be billed to cover the remaining balance and reduce the financial burden on the patient.
It is crucial for billers to carefully review the primary insurance EOB to identify any gaps in coverage. They should pay close attention to the services or treatments that are excluded, have limited coverage, or require prior authorization. By identifying these coverage gaps, billers can work with the secondary insurance to ensure proper reimbursement and minimize out-of-pocket costs for the patient.
Billing secondary insurance for coverage gaps not only benefits the patient but also optimizes the reimbursement process for healthcare providers. It allows for a more comprehensive and efficient reimbursement process, ensuring that patients can access the necessary healthcare services without excessive financial burdens.
Scenario 3: Coordination of Benefits
In the realm of primary and secondary insurance, coordination of benefits (COB) plays a critical role in determining when to bill secondary insurance. COB refers to the process of determining how multiple insurance plans work together to cover medical expenses for an individual who is covered under more than one policy.
When an individual has both primary and secondary insurance policies, it is essential for billers to understand and follow the specific COB rules and guidelines set by the insurance companies. These rules outline the order in which the insurance policies should be billed and how they should coordinate their payments.
The primary insurance is typically billed first, and it covers a portion of the medical expenses according to the policy’s terms and conditions. Once the primary insurance has processed the claim and paid its share, billers can then submit the remaining balance to the secondary insurance for potential reimbursement.
However, the COB process may vary depending on the specific rules set by the insurance companies. Some secondary insurance policies require that the primary insurance submit the claim first before they process any payments. In these cases, the biller should bill the primary insurance initially, and once the primary insurance has paid its share, they can then submit the remaining balance to the secondary insurance.
Alternatively, some secondary insurance policies may have a “non-duplication of benefits” policy. This means that they will only pay out if the primary insurance’s payment is less than what they would have paid if they were the primary insurance. In these instances, billers should coordinate with both the primary and secondary insurance companies to ensure proper billing and reimbursement.
Coordination of benefits becomes crucial in avoiding overpayment from the insurance companies and preventing the insurance coverage from exceeding the total cost of the medical service. It requires clear communication and collaboration between billers, insurance companies, and patients to ensure accurate billing and optimal reimbursement.
Understanding the COB rules specific to each insurance policy is imperative for billers to effectively determine when to bill secondary insurance. By adhering to these guidelines, billers can ensure proper reimbursement, avoid any billing errors, and minimize the financial burden on patients.
Conclusion
Knowing when to bill secondary insurance is crucial for healthcare providers and billers to maximize reimbursement and minimize financial burdens on patients. By understanding primary and secondary insurance, as well as the scenarios that call for billing secondary insurance, healthcare providers can ensure proper utilization of insurance policies and optimize the revenue cycle.
Primary insurance serves as the first line of coverage and covers a portion of the medical expenses. Secondary insurance acts as a safety net, covering any remaining balance not covered by the primary insurance. The interplay between primary and secondary insurance is essential to ensure comprehensive coverage and minimize out-of-pocket costs for patients.
There are several situations in which billers should consider billing secondary insurance. These scenarios include deductibles and co-payments, coverage gaps, and coordination of benefits. When patients have deductible or co-payment obligations, the biller should bill the secondary insurance to minimize the patient’s financial burden. Coverage gaps in the primary insurance policy should be identified, and the secondary insurance can be billed to fill those gaps. Coordination of benefits determines the order in which insurance policies are billed, ensuring proper reimbursement without exceeding the total cost of the medical service.
Proper understanding of these scenarios enables billers to accurately identify when secondary insurance should be billed. This not only benefits patients by reducing their out-of-pocket costs but also ensures optimal reimbursement for healthcare providers. By effectively coordinating with both primary and secondary insurance companies, billers can facilitate a seamless reimbursement process and provide financial relief to patients.
In conclusion, healthcare providers and billers must familiarize themselves with the intricacies of primary and secondary insurance and know when to bill secondary insurance. By doing so, they can navigate the complex insurance landscape, provide comprehensive care to patients, and optimize the financial aspect of healthcare services.